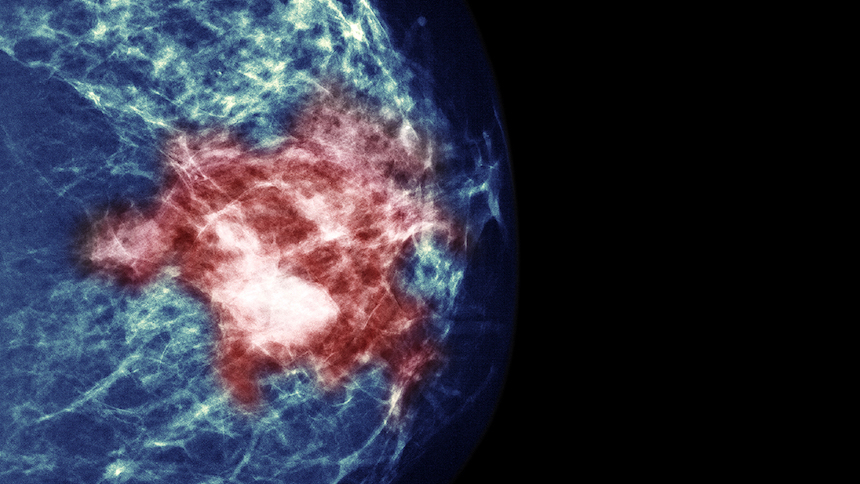
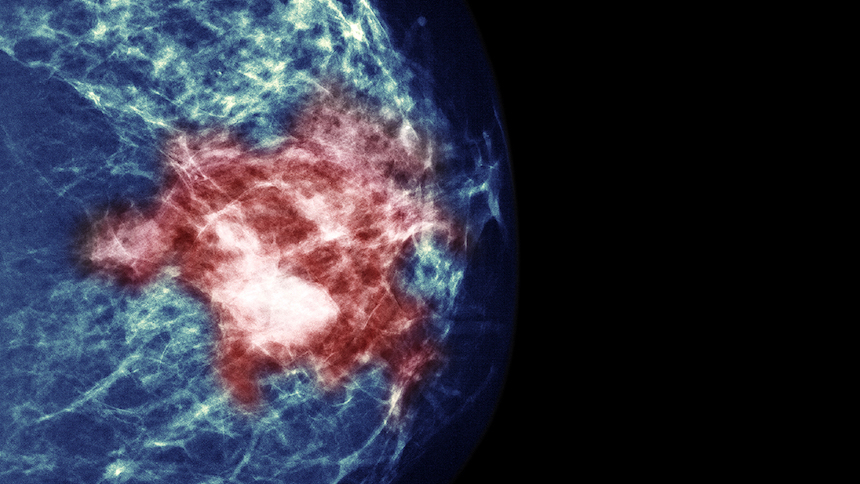
The Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) has established a new milestone in evidence-based treatment for early breast cancer. Through longstanding collaboration, mutual trust, and data transparency, they have gathered individual patient data for 4756 women randomly allocated in ten trials to either neoadjuvant chemotherapy (NACT) or adjuvant chemotherapy, with a median follow-up of 9 years (IQR 5–14). The results of this meta-analysis, published in The Lancet Oncology, substantiate that NACT results in higher rates of breast-conserving therapy than does adjuvant chemotherapy (rate ratio 1·28 [95% CI 1·22–1·34]), without compromising on distant recurrence, breast cancer survival, or overall survival.
Much emphasis is given by the authors to an increase in local recurrence in the NACT group (15 year absolute increase of 5·5% [95% CI 2·4–8·6]). Whether NACT itself could be held accountable for the small increase in local recurrences is questionable. Higher local recurrence with breast-conserving surgery than with mastectomy is inherent to breast-conserving therapy. The meta-analysis by Mieog and colleagues showed no significant difference in local recurrence between patients receiving breast-conserving surgery after NACT and breast-conserving surgery followed by adjuvant chemotherapy, even with inclusion of those receiving NACT that were initially scheduled for mastectomy.
In the meta-analysis by the EBCTCG, NACT led to response of the primary tumour, which undoubtedly led to concomitant downstaging of the axillary lymph nodes. Unfortunately, the EBCTCG was not able to collect data for lymph node status before and after neoadjuvant treatment in these trials. Moreover, axillary treatment strategies have drastically changed in the last two decades, making interpretation of older findings difficult. Probably for these reasons, downstaging of lymph node status was not discussed in the Article. Axillary lymph node dissection is associated with substantial long-term morbidity and is often considered to be worse than morbidity caused by breast surgery. Studies have shown that pathological complete response (pCR) of the axilla is achieved in 41–75% of patients with HER2-positive or triple-negative cancer receiving NACT. Especially among patients with an ultrasound-positive or cytological-positive axilla who had a clinical response with downstaging to a negative axilla, controversy still exists regarding the timing and accuracy of nodal staging with sentinel lymph node biopsy. Several studies have addressed the accuracy of nodal staging after NACT and current consensus is that sentinel lymph node biopsy after NACT in patients with initial positive axilla is considered accurate if at least three or more sentinel nodes are detected and examined. Although the willingness of surgeons to omit axillary lymph node dissection or radiotherapy of the axilla in patients with complete response to NACT is high, no studies have yet investigated locoregional outcomes. A randomised phase 3 trial is ongoing to assess the role of axillary radiotherapy versus no axillary radiotherapy in patients who converted to pathologically node-negative disease after NACT.
As was shown in the EBCTCG meta-analysis, patients with high-grade, hormone receptor-negative tumours were most likely to achieve a complete clinical response of the primary tumour after NACT. With the introduction of targeted therapies and improved systemic strategies, substantial improvements in pCR have been seen in the past decade, especially in patients with HER2-positive or triple-negative breast cancers. Several trials have reported consistently high pCR proportions of up to 83% among HER2-positive, hormone receptor-negative cancers treated preoperatively with combination chemotherapy and (dual) targeted anti-HER2 agents. These complete responders are offered routine breast cancer surgery similar to patients who did not receive NACT. A consensus statement on the extent of breast cancer surgery after NACT recommends inclusion of only the radiological residual area of the primary tumor. When this recommendation is extrapolated to patients with a radiological complete response, the question is raised as to whether breast surgery could be considered an unnecessary procedure. Safe omission of surgery depends on the ability to identify pCR preoperatively. Obviously, the tumor site should be marked with a clip before initiation of NACT to localize the residual tumor after NACT. Several groups are investigating the accuracy of core needle biopsies in the marked area to establish pCR after neoadjuvant treatment, in either those with radiological complete response (MICRA study; TrialRegister.nl, number NTR6120) or those with HER2-positive or triple-negative disease with partial or complete response (NCT02455791). On the basis of initial findings of high accuracy of core needle biopsies in small studies, single-arm studies have started recruitment to establish long-term outcomes for omission of breast surgery (NCT02945579).
With the evidence generated from this meta-analysis, patients with large tumors can be recommended to have NACT and subsequent breast-conserving surgery depending on response assessment. Further studies will tailor the optimum extent of breast and axillary treatment on the basis of response to NACT.