Parents of children with congenital heart disease (CHD) want individualized, formal psychosocial support during their children’s in-hospital stays, according to a new study published in the Journal of Pediatrics. The study by researchers from Nemours Children’s Health System outlines ways to optimize mental health for parents and mitigate the impact of stress on long-term outcomes for children and families.
“The post-surgical recovery period for children with CHD is an incredibly stressful time for parents. Uncertainty, communication challenges, and limited opportunities to engage in self-care can impact their mental health,” said Erica Sood, PhD, senior author and pediatric psychologist within the Nemours Cardiac Center at Nemours/Alfred I. duPont Hospital for Children. “This research helps us understand how we can deliver the psychosocial supports parents need during stressful hospitalizations and after hospital discharge.”
CHD is the most common birth defect, often requiring extensive cardiac surgery in a child’s first year of life. Children with CHD are at high risk for neurodevelopmental and behavioral impairments, and researchers say promoting parental mental health can support positive outcomes for children with CHD and their families.
Using qualitative and quantitative methods to determine parental preferences for the goals and structure of psychosocial programs, researchers interviewed 34 parents (20 mothers and 14 fathers) of 21 young children with CHD. Parents indicated that they want their child’s medical team to support their psychosocial needs at each stage of care. Parents wanted psychosocial support to meet their unique needs through individualized programs delivered by nurses, physicians, psychologists, social workers, and peer mentors.
Past research has shown that during hospitalizations for CHD, parents’ normal roles and responsibilities are interrupted by the level of intense care their child needs and that a lack of formal guidance on how parents can care for their critically ill child can contribute to anxiety, depression, and acute stress. Psychosocial interventions can benefit parents’ mental health and improve children’s outcomes, but can be difficult to implement during hospitalization.
“Parental mental health programs are a critical component of CHD care to influence children’s health outcomes, and families are interested in receiving this care in ways that support where they and their child are in their healing journey,” said Colette Gramszlo, PhD, lead author and a pediatric psychology fellow at Nemours/Alfred I. duPont Hospital for Children. “Hospitals should establish a formal process for offering this assistance to facilitate improved care, coordination and communication.”
Parents recommended that psychosocial interventions should:
1) support their partnership in their child’s care,
2) promote their own self-care,
3) facilitate communication with providers,
4) prepare parents for challenges after hospitalization,
5) provide education about child neurodevelopment, and
6) help parents engage social support.
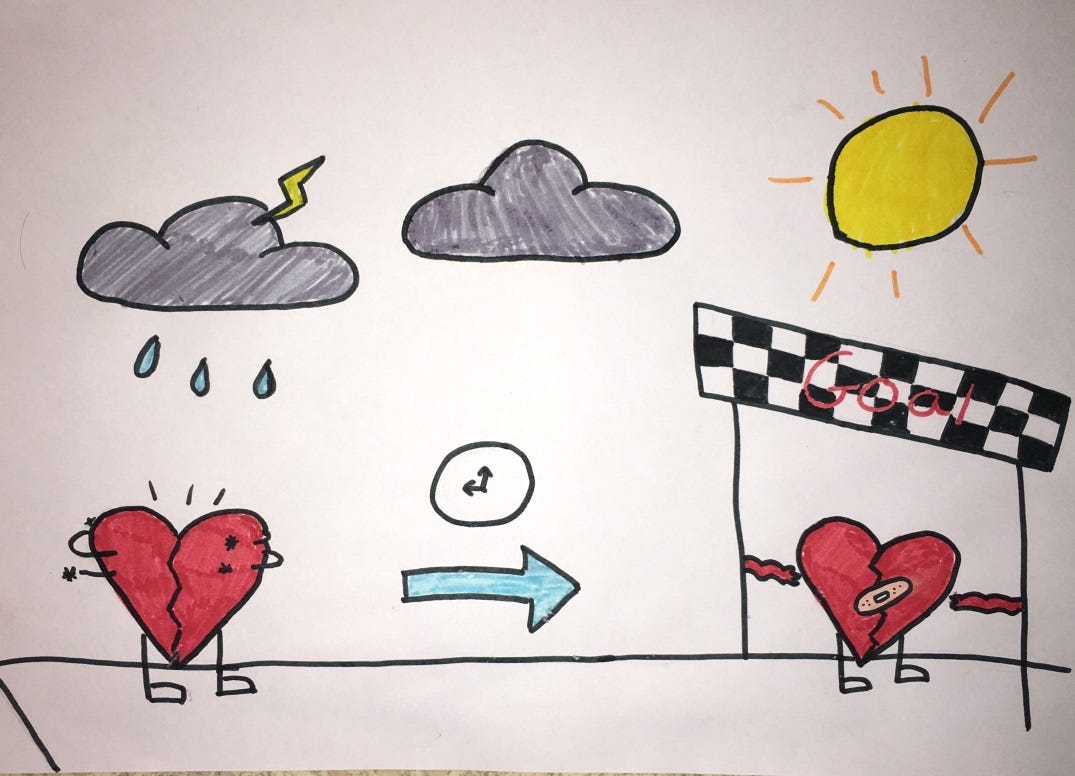
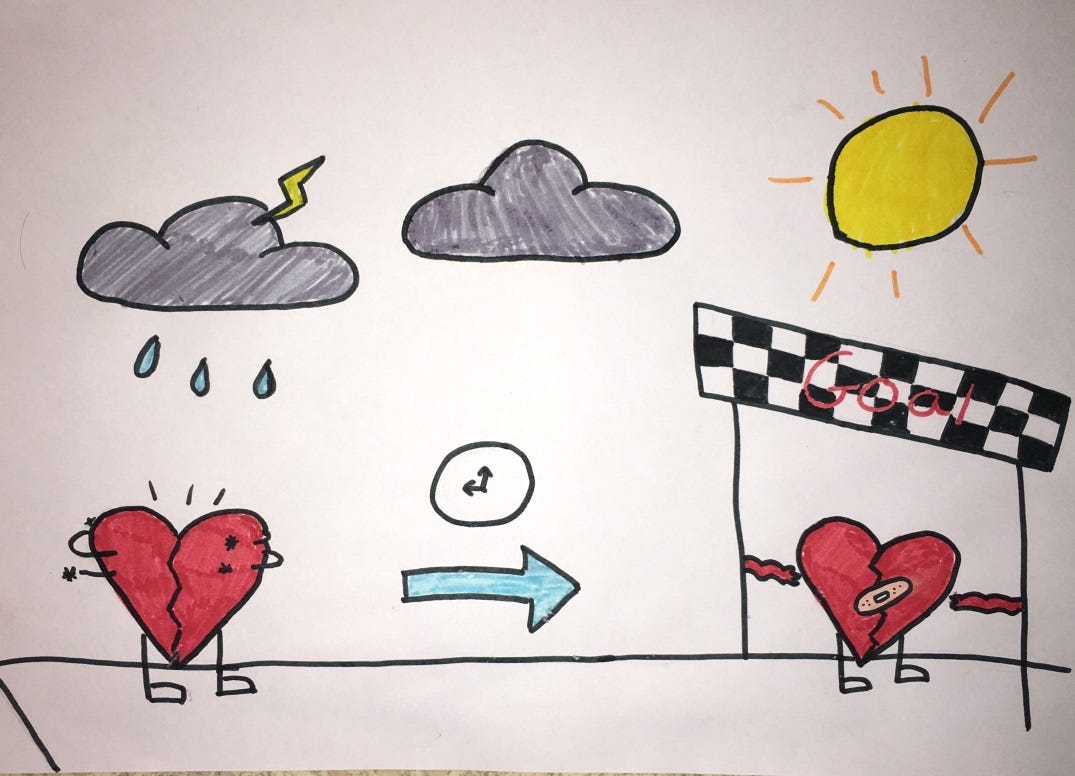
As a result of this research, Nemours Cardiac Center recently developed and tested a bedside tool to promote formal parent education and support in caring for their critically ill child. The tool provides a visual aide to empower parents to participate in their child’s care through safe and developmentally appropriate activities.


After my Coronary Artery Disease (CAD) diagnoses, I was immediately advised for a coronary angioplasty, then a stent. After a while my condition got worse again with severe shortness of breath and angina, so i started on a natural CORONARY ARTERY DISEASE (CAD) TREATMENT from Herbal Health Point, the herbal treatment was very effective treating my heart condition and the shortness of breath. I had a total decline in symptoms. Visit their web page ww w. herbalhealthpoint. c om. Its been 2 years since the treatment, I do lots of walking and lost some weight. My daughter also used their CHF product for her congestive heart failure, very effective.