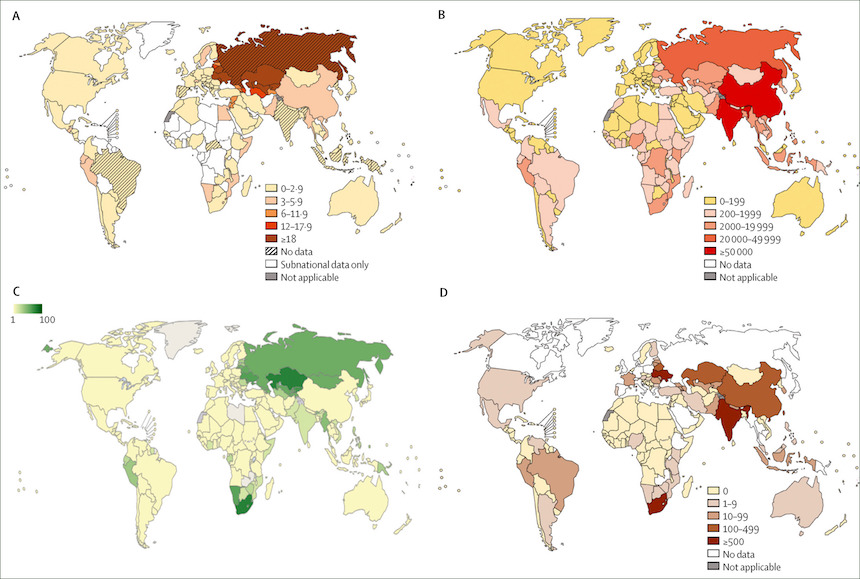
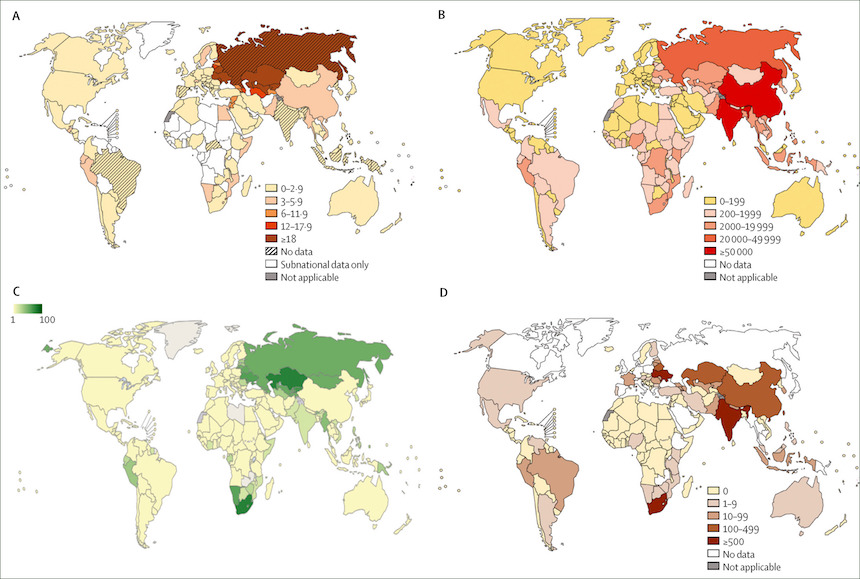
(A) The percentage of new tuberculosis cases that are MDR. (B) Estimated number of cases of MDR tuberculosis in diagnosed patients with pulmonary tuberculosis. (C) Incidence of MDR tuberculosis and rifampicin-resistance per 100 000 individuals of the general population. Available from www.who.int/tb/data. (D) Number of patients with confirmed XDR tuberculosis who started treatment in 2014. Parts (A), (B), and (D) are from the WHO Global Tuberculosis Report, 20151. MDR=multidrug resistant. XDR=extensively drug resistant.
The global mission to reduce the number of new tuberculosis (TB) cases face critical challenges as multidrug-resistant (MDR) and extensively drug-resistant (XDR) tuberculosis go undetected in countries where at-risk communities have little to no access to drug testing. A new report from the Lancet medical journal claims one in five TB cases are now resistant to at least one major anti-TB drug. Roughly 5 percent of all cases are considered “multi drug-resistant” to two vital first-line drugs, isoniazid and rifampicin, or “extensively drug-resistant” to fluoroquinolones and second-line injectable drugs as well.
The World Health Organization (WHO) has branded TB the “world’s top infectious disease killer,” taking 5,000 lives each day. In 2015, an estimated 1.8 million people died from TB related illnesses and the disease is the leading killer of HIV-positive people- in 2015, 35 percent of HIV deaths were due to TB.
The spread of drug-resistant TB is especially deadly with MDR TB having a 40 percent mortality rate and 60 percent for XDR TB. Drug-resistant TB is also costly, making up just 5 percent of all cases, but MDR TB accounted for a third of the $6.3 billion allocated for the global response to TB in 2014. Unsurprisingly, “the heaviest burden is carried by communities which already face socio-economic challenges: migrants, refugees, prisoners, ethnic minorities, miners and others working and living in risk-prone settings, and marginalized women, children and older people,” the WHO said in a press release Wednesday, announcing a new set of ethics guidelines for TB patients.
Humanosphere reports that researchers originally thought drug-resistant TB was less transmissible- mostly acquired by patients who did not fully comply with treatment regimens, but recent studies show that as many as 95.9 percent of new TB cases infected with multi drug-resistant strains were spread from person-to-person. Migration and travel is supporting the spread of these strains. In 2015, about half of the world’s estimated 480,000 cases of new MDR TB cases were in India, China, and Russia.
Funding for detection and treatments will help curb further spread of TB but an October 2016 report by the Treatment Action Group notes that TB research and development funding in 2015 fell by $53.4 million from 2014, to its lowest point since 2008. For the first time in more than five decades, new anti-TB drugs were approved and released in 2012 and 2013, but access to those drugs is limited in communities where they are needed the most. Dr. Zhenkun Ma, lead author for Global tuberculosis drug development pipeline: the need and the reality, concluded that the pipeline of new drugs for TB under clinical development is not considered to be a very extensive drugs “pipeline” for such a major disease as TB.
Furthermore, patients are often infectious for months before they seek care. Employing mobile clinics and low cost testing equipment will help healthcare workers find, diagnose, and treat patients before they seek clinics themselves- a technique called active case finding. However, even when healthcare workers and at-risk communities are proactive in screening for TB, most diagnostic tests in at risk-communities can not detect drug-resistant TB or will only detect resistance to one drug. Keertan Dheda, lead author of the Lancet report and professor of medicine at the University of Cape Town told Humanosphere that “the best way to deal with drug-resistant TB is to deal with TB itself” by addressing the major drivers such as property and overcrowding, HIV, cigarette smoke, and exposure to biomass fuels that weakens people’s immune systems.

