Mosquito-borne diseases claim millions of lives each year- in 2015, there were roughly 212 million malaria cases and an estimated 429,000 malaria deaths. Testing for mosquito-borne viruses requires devices that are approximately the size of a microwave oven and can cost up to $20,000. The viruses are especially dangerous in poor countries where clinics have limited access to the diagnostic tools needed for quick testing.
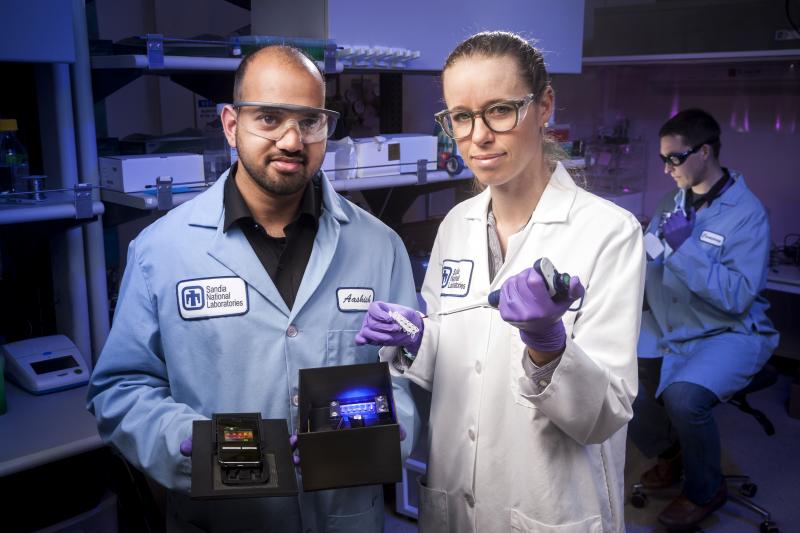
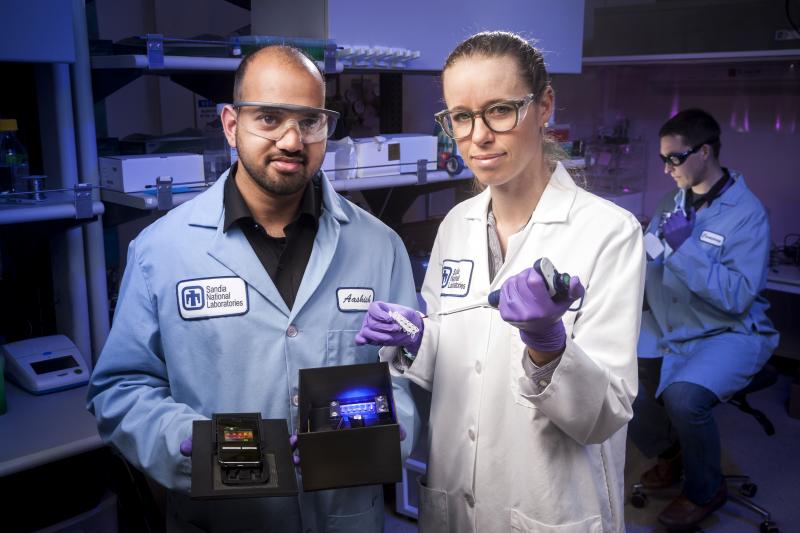
Researchers at Sandia National Laboratories have developed a portable battery-powered device that costs as little as $100 and is operated by a smartphone to test patient samples for chikungunya, Zika, and dengue within thirty minutes. The Sandia team describes the device in a paper published in Scientific Reports.
“This idea came together through a couple of different strands from other projects,” said Robert Meagher, lead researcher of the project and chemical engineer at Sandia, to R&D Magazine. “The first one is still ongoing but we were trying to field-based detection of viruses from a surveillance point of view. The next ones were building automation to improve vector surveillance and create simple robust assays that didn’t require as much human labor or sample prep.”
Samples are placed in a storage container that uses the loop-mediated isothermal amplification (LAMP) diagnostic method, a technique that eliminates the need to process biological samples before testing, while also being able to replicate DNA/RNA without power-intensive heating and cooling cycles.
Another element of this technology is a technique called quenching of unincorporated amplification signal reporters (QUASR), which involves labeling synthesized viral DNA fragments as primers with fluorophores or molecules that emit bright light signals. Primers incorporate into heated and amplified DNA samples and QUASR causes samples that contain viral DNA/RNA to appear bright, while negative reactions remain dark.
“We designed the chemistry of the assays so each well gives off a distinct signal,” said Meagher. “Zika and Chikungunya will emit a red indicator while the second well will generate a green signal for Dengue.”
“Dengue was the probably the most challenging because it is comprised of four different viruses and has more genetic diversity than other pathogens due to how widespread it is around the globe,” he continued, noting that the team needed to develop an assay to detect all four strains of dengue in a single reaction.
Users will then place a smartphone over the container to act as a fluorimeter— a device that measures the fluorescent light emitted from samples at different wavelengths. This triggers a mobile app that begins sample analysis in a three-step process.
First the program activates assay incubation and turns on a hotplate. This causes mixing of the sample with dried ingredients and other chemicals for thirty minutes.
Then, at the culmination of the testing period, Sandia’s software takes a picture of the sample, and finally—conducts an analysis of the image.
“The camera spits out an array of pixels with different intensity, taking that data and transforming it into the chromo luminescence space so users can avoid false positives,” explained Meagher.
Health workers using this device would be able to provide a diagnosis of the infection based on the color and brightness of the fluorescence. This resolution could provide greater detection certainty than the naked eye of a lab technician.
Meagher notes that this device has many field applications and could benefit clinics in remote areas. “It makes an impact in allowing clinicians to quickly do diagnostic on the spot and get results back to the patient the same day. Instead of relying on a centralized laboratory, this could streamline cheap portable instruments that can test patients on the spot,” Meagher added.
Health workers could implement this test at their clinics for a relatively low cost, and according to the Sandia research team—the cost of the phone they used for testing was $20.
The project is still in beta mode, but according to Meagher this device would ideally be tested in an area where one or more of the diseases are currently circulating, while providing support and training to local inhabitants so they know how to use the app.
According to Meagher, there will always be a need for new cures and complementary diagnostics, but he elaborated that one of the challenges with this type of research is that it is done after the outbreak has already occurred. Ongoing basic research needs to continue in order to better predict and prevent outbreaks, he continued, explaining that an added benefit of this device is that it offers an opportunity to conduct experiments that can be rigorously evaluated.

