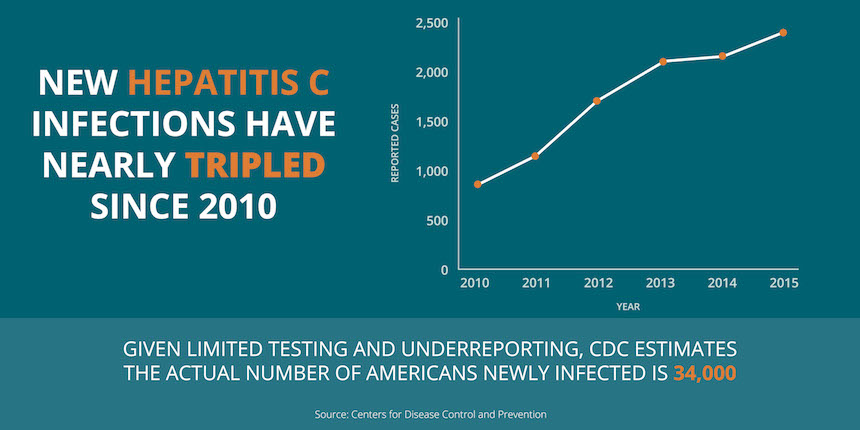
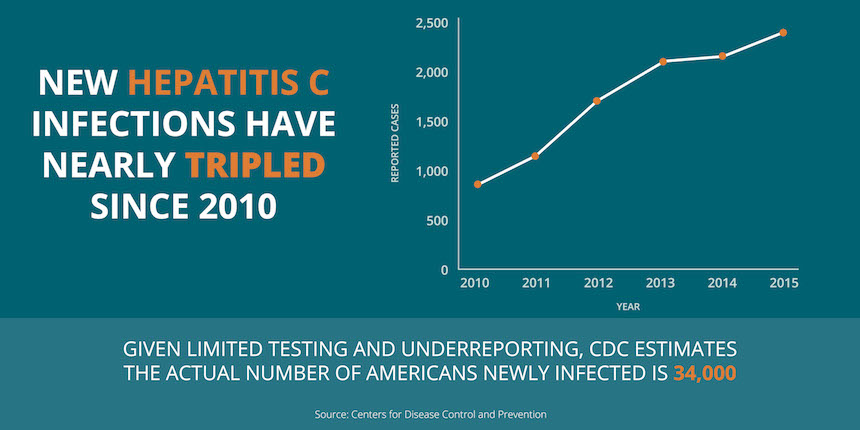
Over just five years, the number of new hepatitis C virus infections reported to CDC has nearly tripled, reaching a 15-year high, according to new preliminary surveillance data released today by the Centers for Disease Control and Prevention (CDC).
Because hepatitis C has few symptoms, nearly half of people living with the virus don’t know they are infected and most new infections go undiagnosed. Further, limited surveillance resources have led to underreporting, meaning the annual number of hepatitis C virus cases reported to CDC (850 cases in 2010 and 2,436 cases in 2015) does not reflect the true scale of the epidemic. CDC estimates about 34,000 new hepatitis C infections actually occurred in the U.S. in 2015.
Hepatitis C kills more Americans than any other infectious disease reported to CDC. The data released today indicate that nearly 20,000 Americans died from hepatitis C-related causes in 2015, and the majority of deaths were people ages 55 and older.
“By testing, curing, and preventing hepatitis C, we can protect generations of Americans from needless suffering and death,” said Jonathan Mermin, M.D., director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. “We must reach the hardest-hit communities with a range of prevention and treatment services that can diagnose people with hepatitis C and link them to treatment. This wide range of services can also prevent the misuse of prescription drugs and ultimately stop drug use – which can also prevent others from getting hepatitis C in the first place.”
Hepatitis C spreading rapidly in new generations, but boomers bear biggest burden
New hepatitis C virus infections are increasing most rapidly among young people, with the highest overall number of new infections among 20- to 29-year-olds. This is primarily a result of increasing injection drug use associated with America’s growing opioid epidemic.
However, the majority (three-quarters) of the 3.5 million Americans already living with hepatitis C are baby boomers born from 1945 to 1965. Baby boomers are six times more likely to be infected with hepatitis C than those in other age groups and are at much greater risk of death from the virus.
While surveillance data do not accurately capture hepatitis C infection rates among infants, other recent CDC studies indicate that hepatitis C virus infections are growing among women of childbearing age – putting the youngest generation of Americans at risk. Hepatitis C treatment not only cures the vast majority of people living with the virus, but also prevents transmission to their partners and children.
Urgent need for expanded testing, treatment, and prevention
Comprehensive approaches are needed to combat the dual epidemics of opioid addiction and injection-related infectious diseases. The U.S. Department of Health and Human Services (HHS) has brought five specific strategies to fight against the opioid epidemic that will save lives and reduce the impact of injection-related infectious diseases. These are: improving access to treatment and recovery services, promoting use of overdose-reversing drugs, strengthening our understanding of the opioid epidemic through better public health surveillance, providing support for cutting-edge research on pain and addiction, and advancing better practices for pain management. Comprehensive syringe service programs (SSPs) are one of many tools that communities can use to prevent hepatitis and other injection-related infectious diseases. These programs also help link people to treatments to stop drug use, testing for infectious diseases that can be spread to others, and medical care.
Two recent CDC analyses provide data to support communities in expanding access to SSPs, should they decide to implement this tool, where it is consistent with local laws. One study indicates that 80 percent of young people with hepatitis C live more than 10 miles from an SSP. Another study published in today’s issue of CDC’s Morbidity and Mortality Weekly Report (MMWR), examines the range of state laws that can influence access to both SSPs and curative treatment for hepatitis C. The study finds that only three states have laws that support full access to both comprehensive SSPs and hepatitis C-related treatment and preventive services for people who inject drugs.
While new medicines can now cure hepatitis C virus infections in as little as two to three months, many people in need of treatment are still not able to get it. HHS recently released the National Viral Hepatitis Action Plan, 2017-2020 that sets goals for improving prevention, care, and treatment of viral hepatitis and puts the nation on a course toward eliminating new hepatitis infections. The importance of this effort was underscored by the National Academies of Sciences, Engineering and Medicine, which in a recent report concluded that eliminating hepatitis C as a public health threat in the United States is feasible if the right steps are taken.
“Stopping hepatitis C will eliminate an enormous disease and economic burden for all Americans,” said John Ward, M.D., director of CDC’s Division of Viral Hepatitis. “We have a cure for this disease and the tools to prevent new infections. Now we need a substantial, focused, and concerted national effort to implement the National Viral Hepatitis Action Plan and make effective prevention tools and curative treatment available to Americans in need.”

