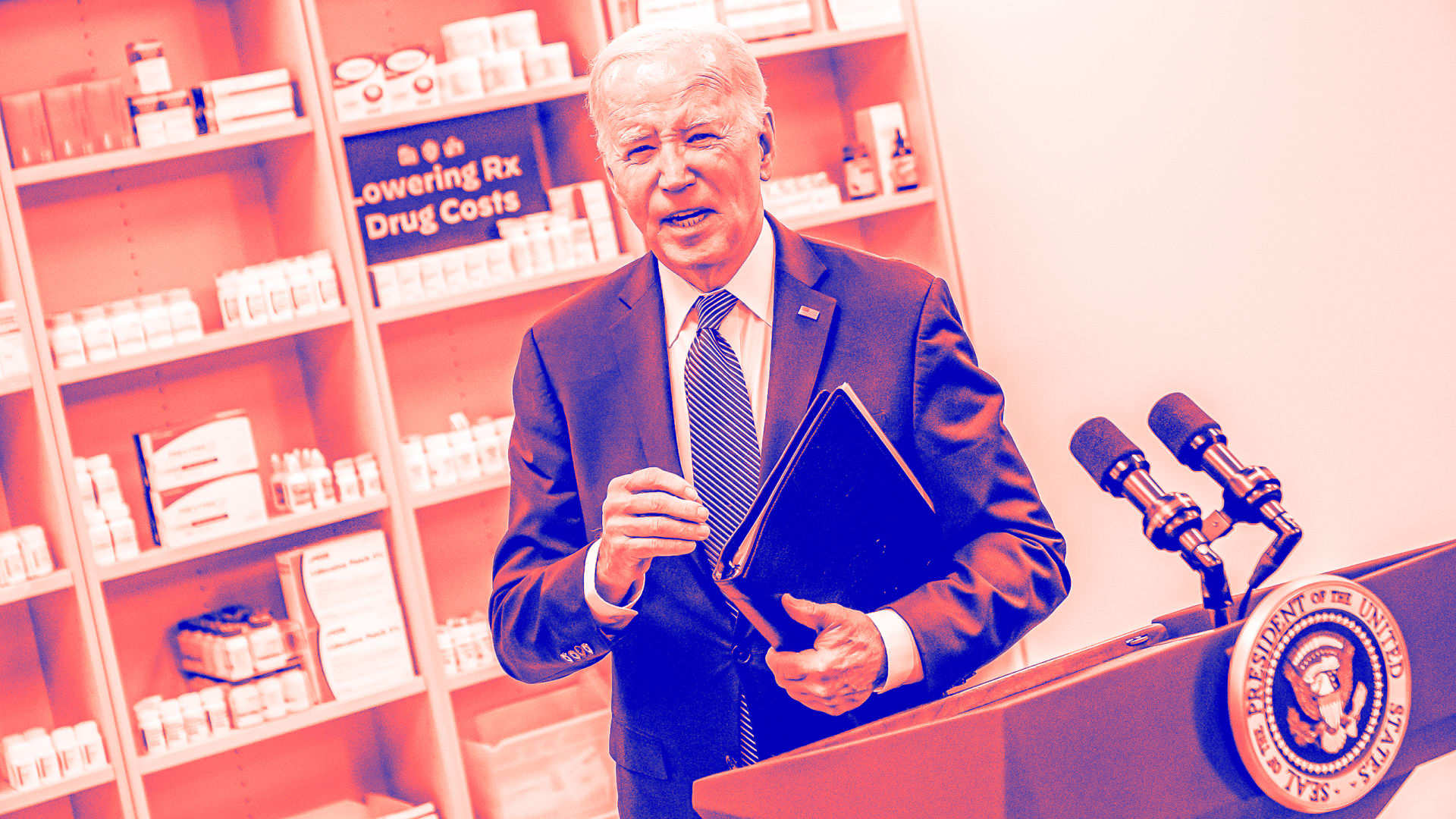
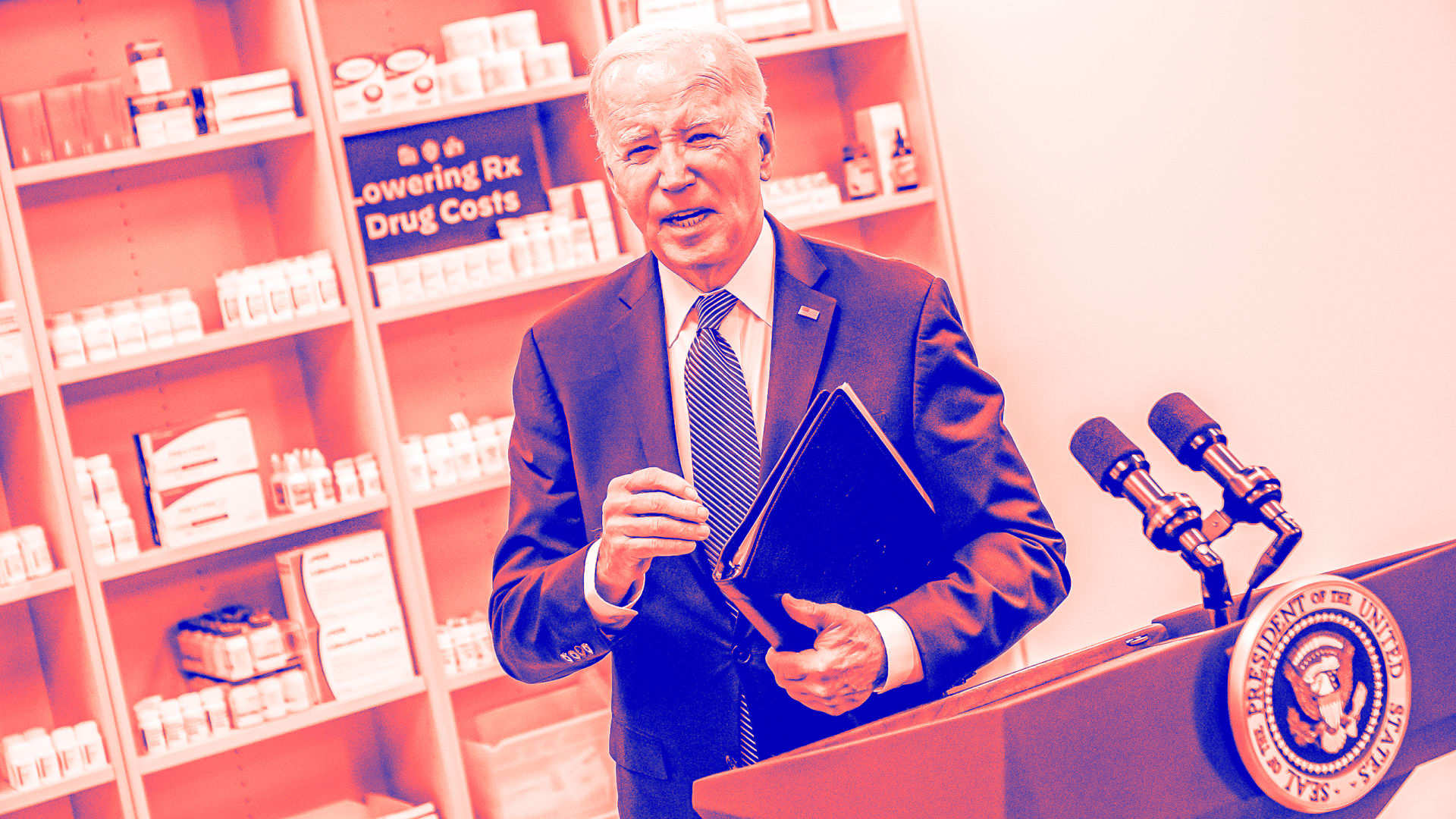
The Biden administration announced on Aug. 16, 2024, the reduced prices of the first 10 drugs it has negotiated with pharmaceutical companies over their Medicare prices.
Provisions authorizing these negotiations were part of the Inflation Reduction Act, which took effect in 2022, but these lower prices aren’t scheduled to take effect until 2026.
The drugs are purchased through Medicare Part D, a prescription drug coverage program for Americans who are 65 and older. The 10 medications were used by 9 million patients with Medicare coverage in 2023, and they accounted for US$56.2 billion in total Medicare spending. Had the negotiated prices been in place that year, the government estimates that Medicare would have saved about $6 billion.
To put this in perspective: Total annual spending on prescription drugs in the U.S. exceeds $405 billion, and Part D alone spends more than $215 billion.
As a scholar who researches the politics of health policy, I remain skeptical that negotiations will end up having an substantial impact on the U.S. health care system in the foreseeable future, even if the law survives ongoing legal and implementation challenges.
At the same time, I do expect that many older adults will reap substantial savings on their out-of-pocket spending on prescription drugs over the coming years. But that will primarily happen due to other Inflation Reduction Act provisions.
Cutting drug costs for Medicare enrollees
The Inflation Reduction Act allows the Centers for Medicare & Medicaid Services to negotiate prices with the companies that make some of the most expensive drugs in the Medicare program, including life-saving cancer and diabetes treatments like Imbruvica and Januvia.
Democrats have hailed these drug pricing provisions as game-changing. Vice President Kamala Harris, who is now running for president, is making efforts to rein in drug prices part of her election campaign.
Former President Donald Trump, however, has been relatively quiet on the issue. Public opinion polls show overwhelming public support for the policy.
Medicare will soon begin to negotiate prices for more drugs, including 30 over the next two years.
If the policy continues to move forward as planned, the drug price negotiation provision is expected to save the U.S. government about $98.5 billion by 2031.
The Biden administration hopes that some of these cost savings will be passed down to Americans 65 and older through reduced Medicare Part D premiums and lower out-of-pocket costs. The White House also hopes to reduce the federal deficit by $237 billion.
Other important benefits for older adults
While negotiations over Medicare drug prices have received the most attention, the Inflation Reduction Act included other provisions that might be even more beneficial for older adults.
These include limiting out-of-pocket spending by older adults on prescription drugs to no more than $2,000 annually by 2025, limiting the growth of Medicare Part D premiums, providing rebates if certain drug price increases outpace inflation, eliminating out-of-pocket costs for vaccines and providing premium subsidies to low-income people 65 and up.


Strong industry resistance, but companies negotiated
Despite their vocal opposition and their ongoing public relations campaign that has attacked this process, all affected U.S. drugmakers decided to engage in the price negotiations.
The daunting alternatives, including paying a penalty that could run as high as 95% of their U.S. pharmaceutical product sales, and a requirement to pull their drugs from the Medicare and Medicaid markets, proved to be strong incentives.
However, the manufacturers of medications have been fighting the measure in court. And despite several losses, this battle will likely continue for the foreseeable future, with uncertain outcomes.
Why US drug prices are so high
Americans pay substantially more for prescription drugs compared with people who live in countries with similar economies. For example, per capita pharmaceutical spending in the U.S. amounted to $1,432 compared to $1,042 in Germany and $766 in France in 2022.
The reasons for this disparity are multilayered and include the overall complexity of the U.S. health care system and the lack of transparency in the drug supply chain. Of course, many other countries also directly set prices for drugs or use their monopoly over health services to drive down costs.
Drug costs impose a big burden on Americans. People who are 65 and older are particularly affected, with 1 in 5 not taking all of their medications as prescribed due to high costs.


Weighing the prospects of price negotiations
In my view, the government’s efforts are a step in the right direction. The potential for real savings for Americans 65 and older will undoubtedly grow as more drug prices are negotiated.
Yet, some real concerns remain.
Even if the negotiated lower prices survive the industry’s legal challenges, it’s possible that future Republican administrations won’t embrace this policy, as Republicans have historically opposed price negotiations for Medicare.
The true effect for patients with Medicare will likely be much smaller than it appears. That’s because the Medicare program and patients often already receive discounts on many of these drugs. These discounts will now be eliminated.
In addition, the pharmaceutical industry has a history of skillfully exploiting loopholes that may further limit the financial impact. Manufacturers have already told shareholders that they expect limited impacts on their profits.
It’s also too soon to tell if this is going to be a win for all Americans. It’s possible that Americans who aren’t covered by Medicare may actually see prices go up, even on these same drugs. Working Americans could thus wind up shouldering ever larger burdens to deliver this support for older adults.
Simon F. Haeder, Associate Professor of Public Health, Texas A&M University
This article is republished from The Conversation under a Creative Commons license.

