The epidemic levels of physicians reporting burnout dropped modestly in 2017, according to a study by researchers at the Stanford University School of Medicine, the Mayo Clinic and the American Medical Association.
“Physicians remain at increased risk for burnout relative to workers in other fields, but there is some good news,” said Tait Shanafelt, MD, director of Stanford’s WellMD Center and a national leader in the movement to improve physician well-being. “For the first time, we’re seeing improvement in the prevalence of burnout symptoms in physicians nationally.”
Burnout decreased and satisfaction with work-life integration improved between 2014 and 2017, according to the study. Still, levels of burnout remain markedly higher than in other fields. About 44 percent of physicians reported at least one symptom of burnout, and only about 43 percent reported satisfaction with their work-life integration, which was less than in 2011.
The study is published in Mayo Clinic Proceedings. Shanafelt, who is also a professor of hematology and the Jeanie and Stew Ritchie Professor, is the lead author. Lotte Dyrbye, MD, co-director of the Mayo Clinic physician well-being program, is the senior author.
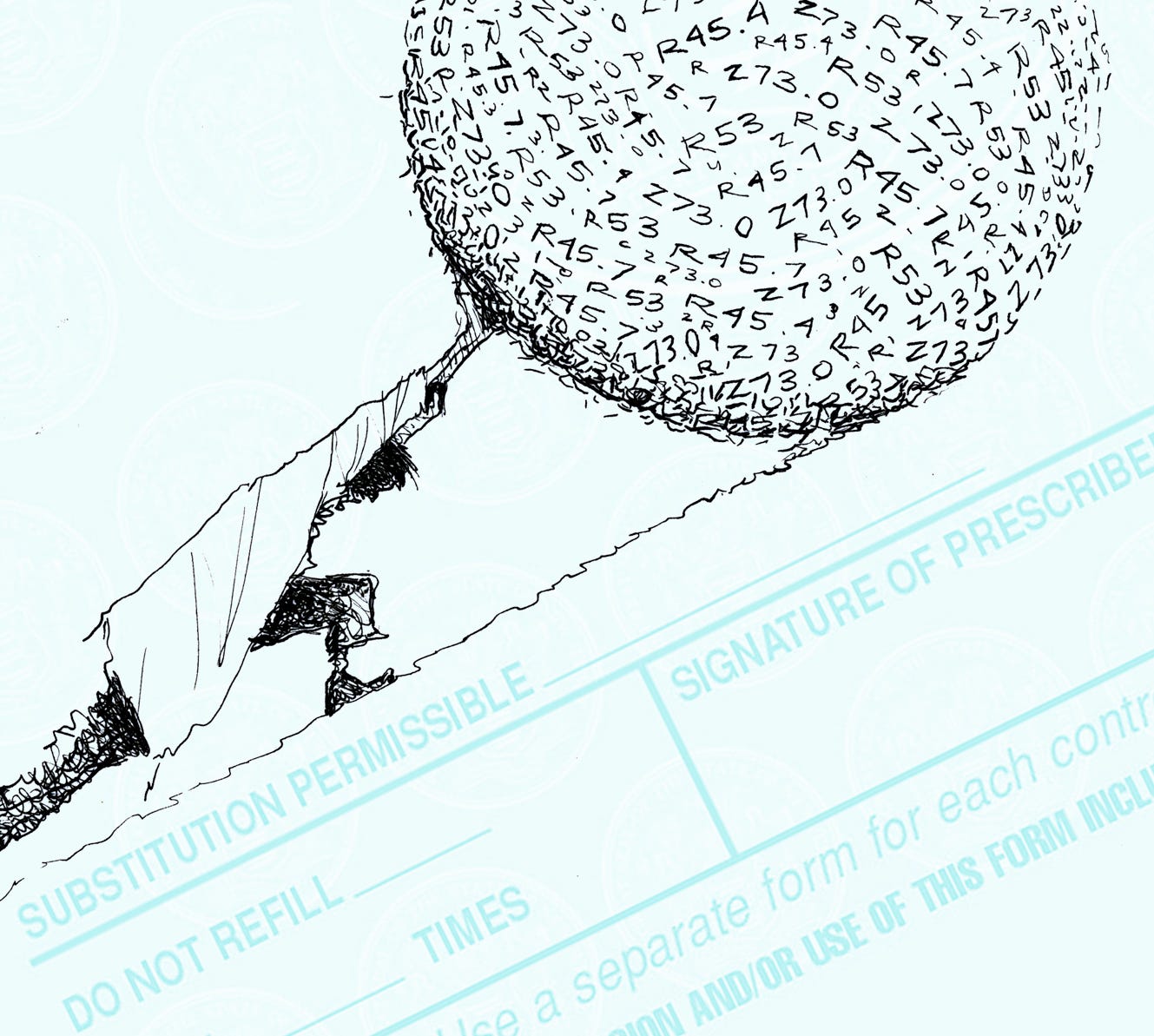
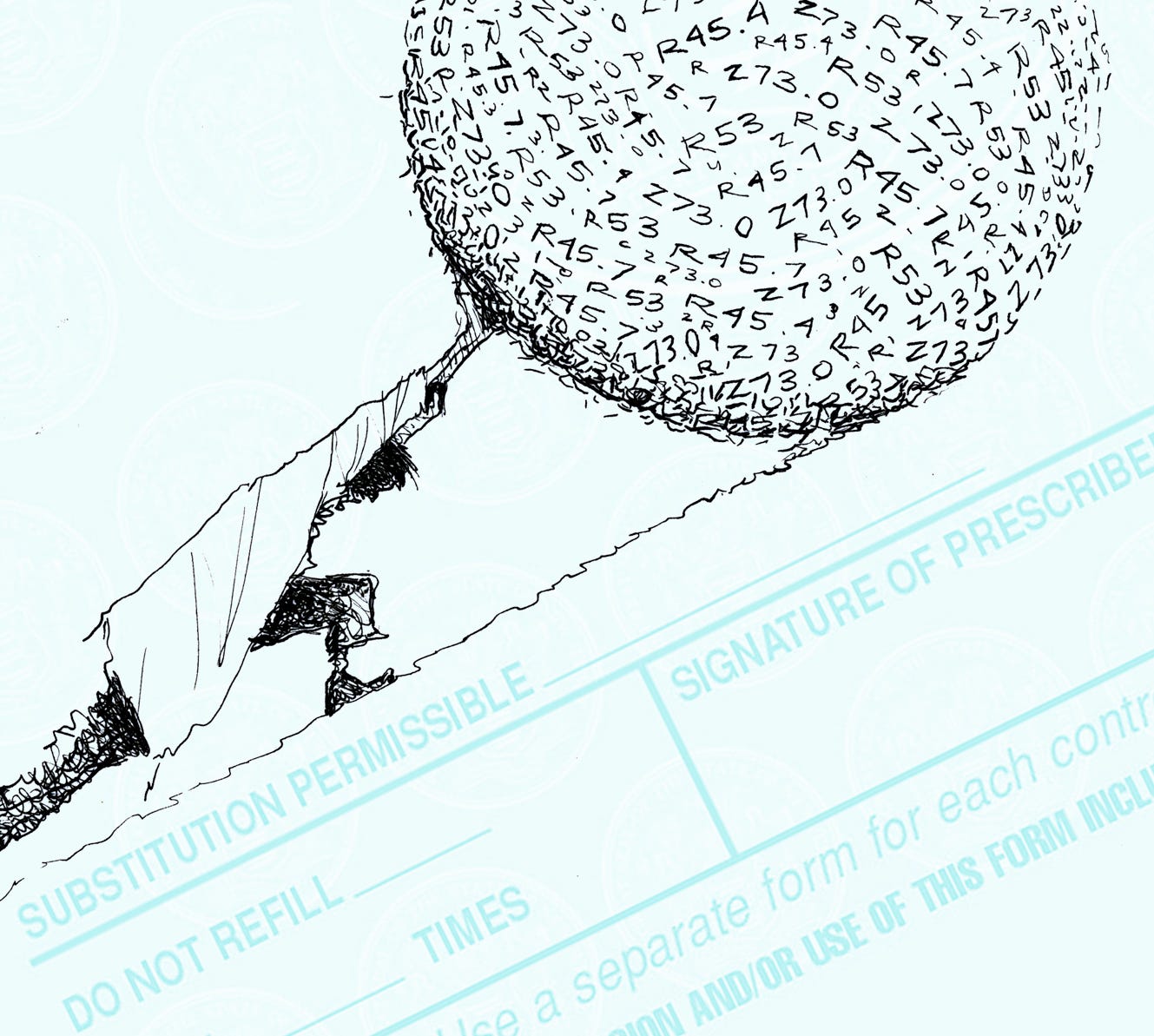
Shanafelt first conducted studies on physician well-being almost two decades ago. Over the years, research uncovered evidence of growing distress and cynicism among physicians due, in part, to spending more time on clerical work at the expense of time spent with patients. Increasing workloads and regulations contributed to high levels of emotional exhaustion and job dissatisfaction. Physicians were leaving their jobs, and their suicide levels were markedly higher than those of other professionals. Still, the studies weren’t being taken seriously enough, Shanafelt said.
“Anytime a study came out on physician burnout, people would say, ‘Well that’s true for all workers. Everybody is stressed out; doctors are no different,'” he said. “There was a need for an ongoing, nationwide study that would compare physicians with other workers in the United States.”
Third in series of national studies
In 2011, while he was at the Mayo Clinic, Shanafelt joined forces with other researchers and the American Medical Association to publish the first of what would be an ongoing series of national studies to measure changes in burnout levels among physicians at three-year intervals. This is the third study in the series; the previous two were conducted in 2011 and 2014. Those studies found that symptoms of burnout were markedly more common in physicians than in workers in other professions, even after adjusting for work hours and other characteristics.
To conduct the current study, researchers sent surveys to a nationwide sampling of physicians and workers in other fields. Among physicians, 5,445, or about 17 percent, completed the survey. Of these, 43.9 percent reported at least one symptom of burnout in 2017, compared with 54.4 percent in 2014 and 45.8 percent in 2011. Symptoms of burnout among workers in other fields remained the same — about 28 percent.
The improvement from 2014 to 2017 in symptoms indicating burnout were not seen among physicians in all specialties, the study reported. Levels among certain specialties, including general surgery and obstetrics and gynecology, failed to show any significant reduction in 2017. Also, the proportion of physicians screening positive for depression showed a modest but steady increase in the three studies: 38.2 percent in 2011, 39.8 percent in 2014 and 41.7 percent in 2017.
The researchers could only speculate about what may have contributed to the decrease in burnout levels in 2017. One possibility is that a large number of burned-out physicians left the workforce, so they were no longer included in the study. Another possibility is that 2014 may have been a particularly challenging time for physicians due to consolidation of hospitals and medical groups, a number of new regulatory factors, and increased administrative burdens. But Shanafelt is hopeful that growing national efforts by government agencies, professional organizations and medical institutions to improve working conditions for physicians may be making a difference.
“Over the last couple of years, we have begun to think about the well-being of health care professionals through the lens of the system and practice environment rather than through the lens of personal resilience. There are now large-scale national efforts, as well as efforts at the institutional level in many organizations, to reduce physician burnout and promote physician well-being,” Shanafelt said. “We can’t say for certain, but it’s looking like those efforts may be starting to make a difference.”

