Researchers from the HIV Prevention Trials Network (HPTN) presented results from the HPTN 094 (“INTEGRA”) study at the 2025 Conference on Retroviruses and Opportunistic Infections (CROI) in San Francisco. The main findings from this randomized controlled trial that enrolled persons who inject drugs showed that similar numbers of participants were on medication for opioid use disorder (MOUD) and antiretroviral therapy (ART) for HIV care or prevention at 26 weeks post-randomization either to an intervention arm that provided integrated services with peer navigation in a mobile unit or to an active control arm that received navigation to integrated services at available community agencies only. Findings showed about seven percent of participants in both arms were determined as alive and on MOUD, about 35 percent of participants living with HIV were virally suppressed, and between three percent and five percent on HIV pre-exposure prophylaxis (PrEP) at 26 weeks post-randomization.
“With 90 percent retention of participants, most of whom had unstable housing through the trial, HPTN 094 provided foundational evidence that mobile units and peer navigation are acceptable in confronting structural and systemic barriers that hinder access to care for addiction and HIV, as well as prevention of HIV,” said Dr. Steven Shoptaw, HPTN 094 protocol co-chair and professor in the University of California at Los Angeles (UCLA) departments of Family Medicine, Psychiatry, and Biobehavioral Sciences. “HPTN 094 also provides data on establishing an integrated care model for improving health outcomes among high-risk populations.”
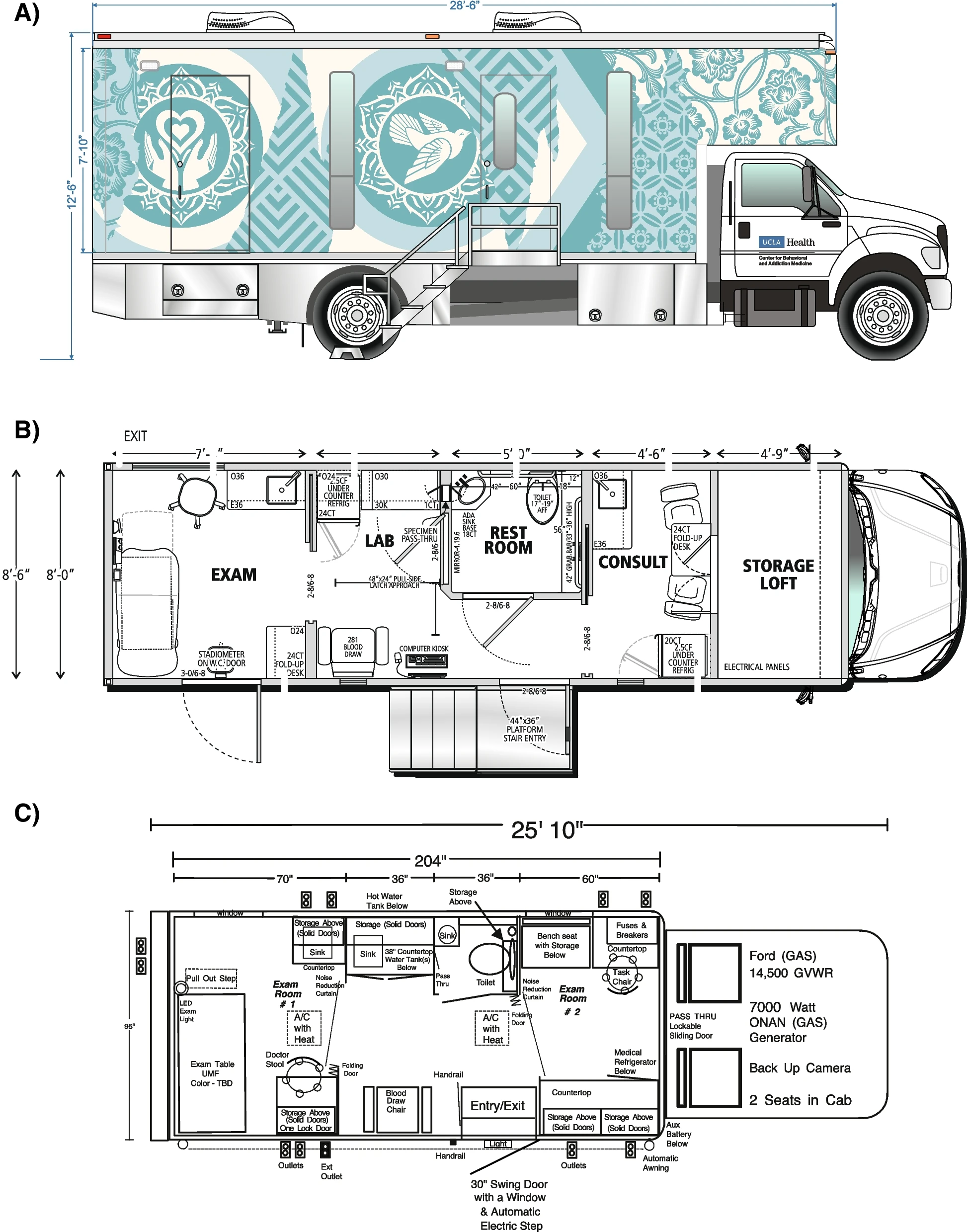
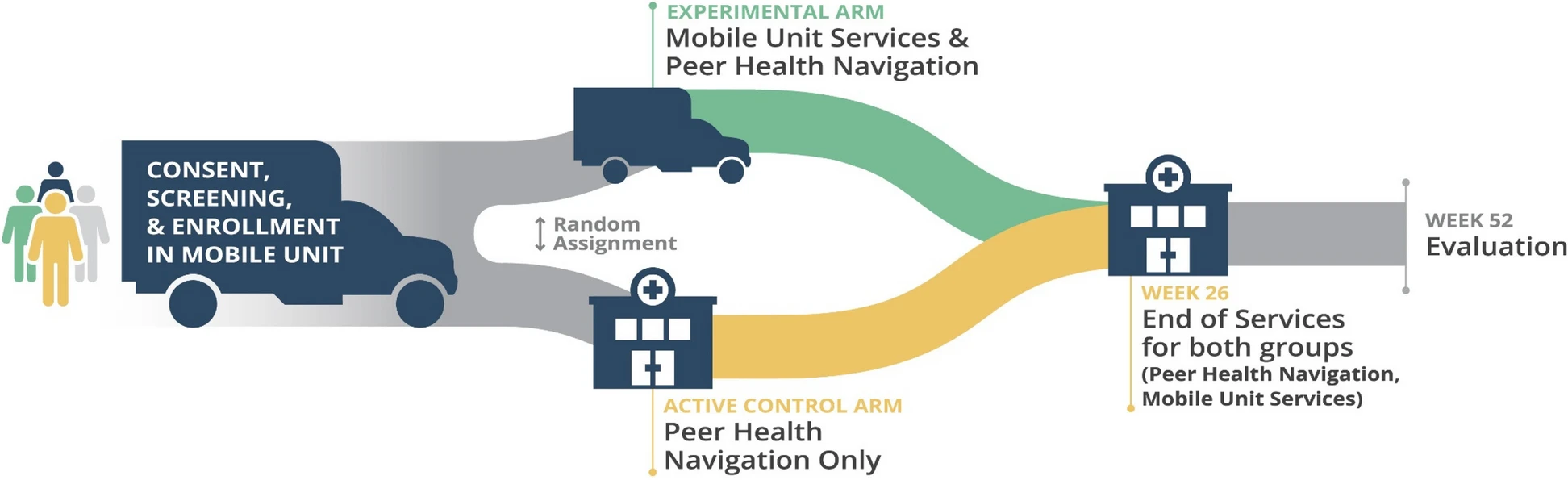
HPTN 094 is the only randomized controlled trial to test the efficacy of using mobile integrated health services for opioid use disorder and HIV prevention or treatment for people who inject drugs. Primary outcomes were being alive at 26 weeks post-randomization, using MOUD, and ART for HIV prevention or care among people who inject drugs in the U.S. By design, this pioneering study tested outcomes when delivering whole-person, integrated strategies using mobile medical units with peer navigation to local services compared to peer navigation to local services alone.
“Opioid use is a critical factor in the lives of people who inject drugs, hindering access to essential health services,” said Dr. Wafaa El-Sadr, HPTN co-principal investigator, director of ICAP, and professor of epidemiology and medicine at Columbia University in New York. “HPTN 094 met people living with opioid use disorder where they are by designing an intervention that brought integrated and judgement-free health, supported by peer navigation.”
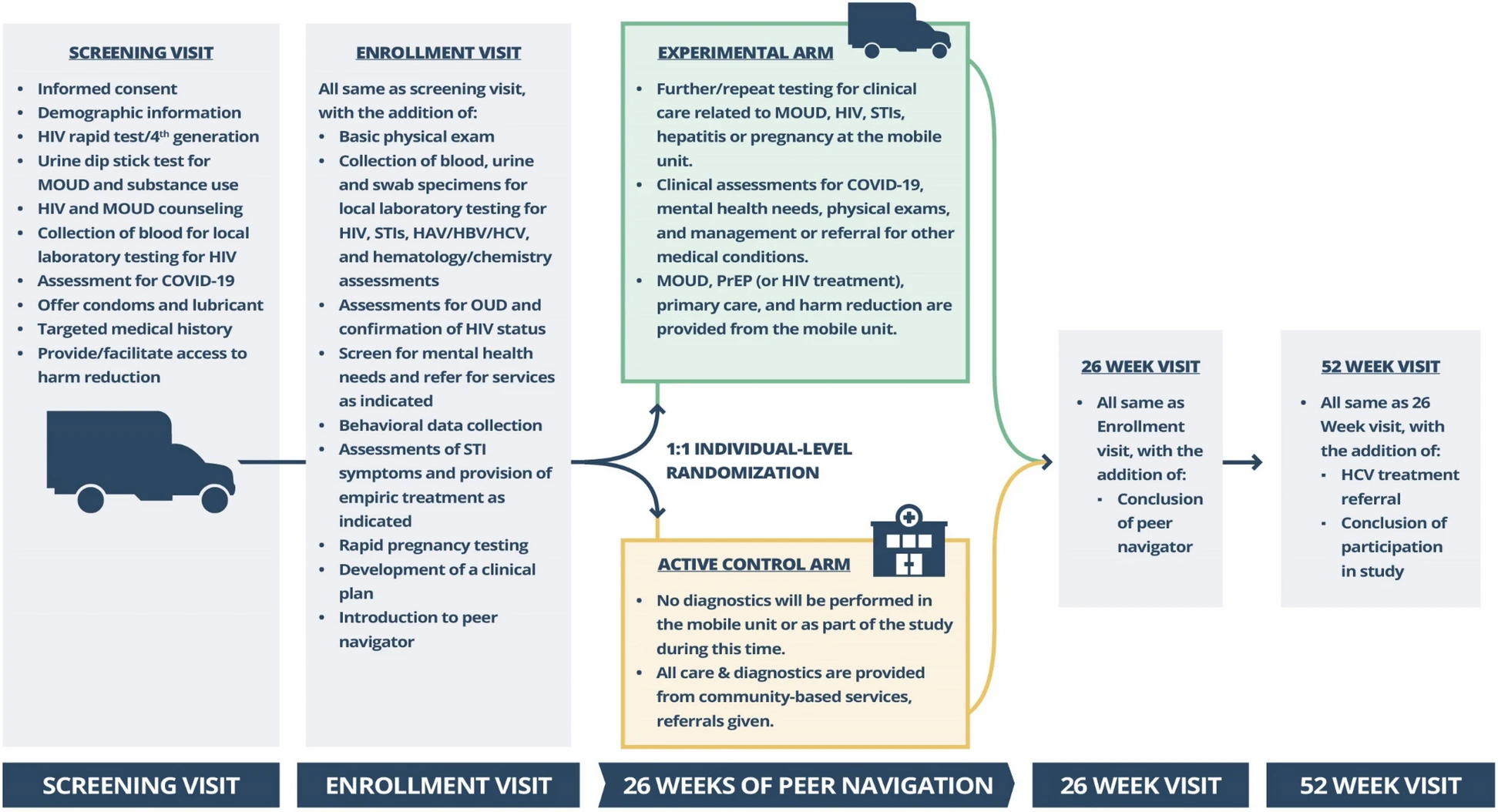
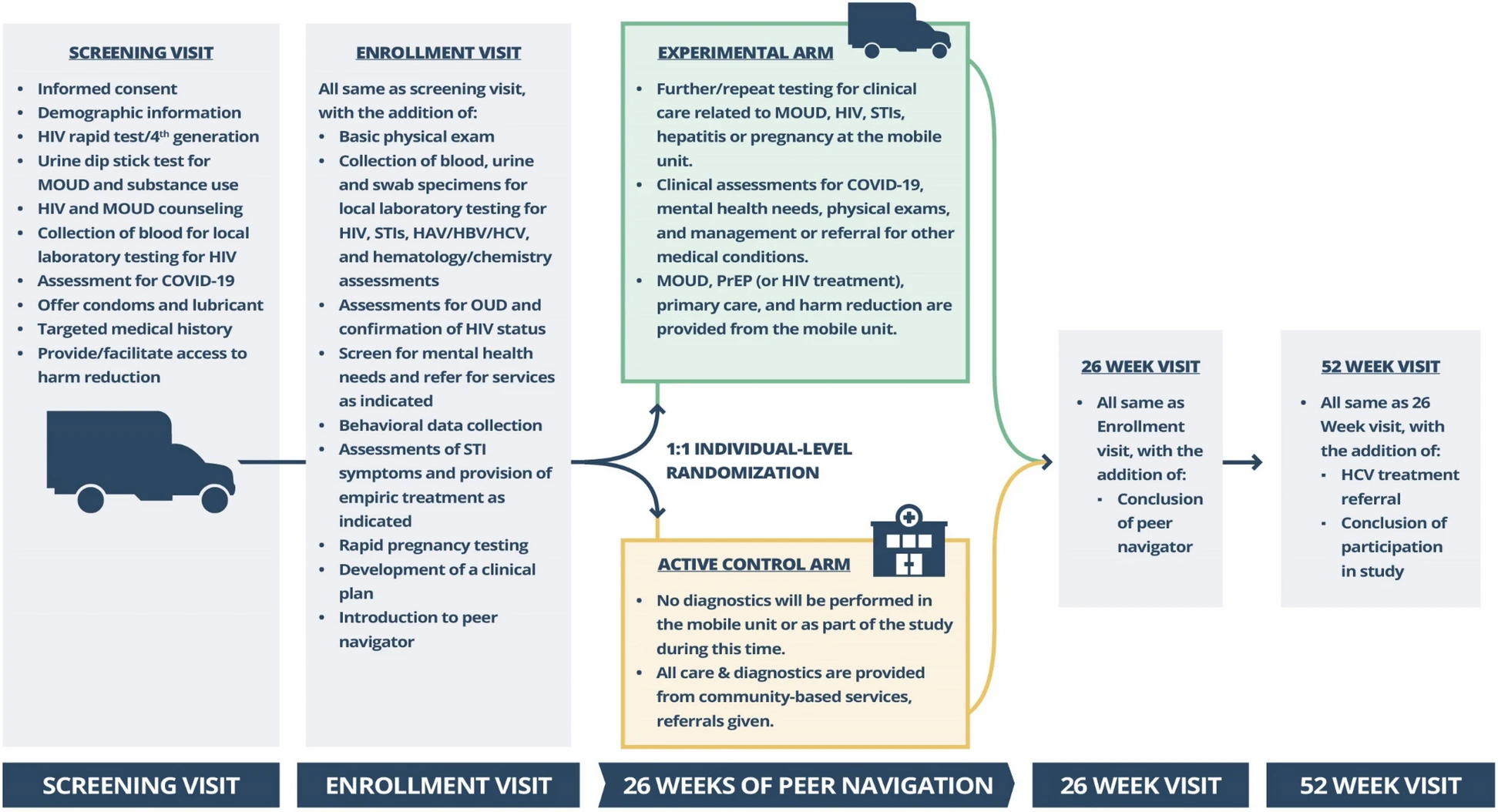
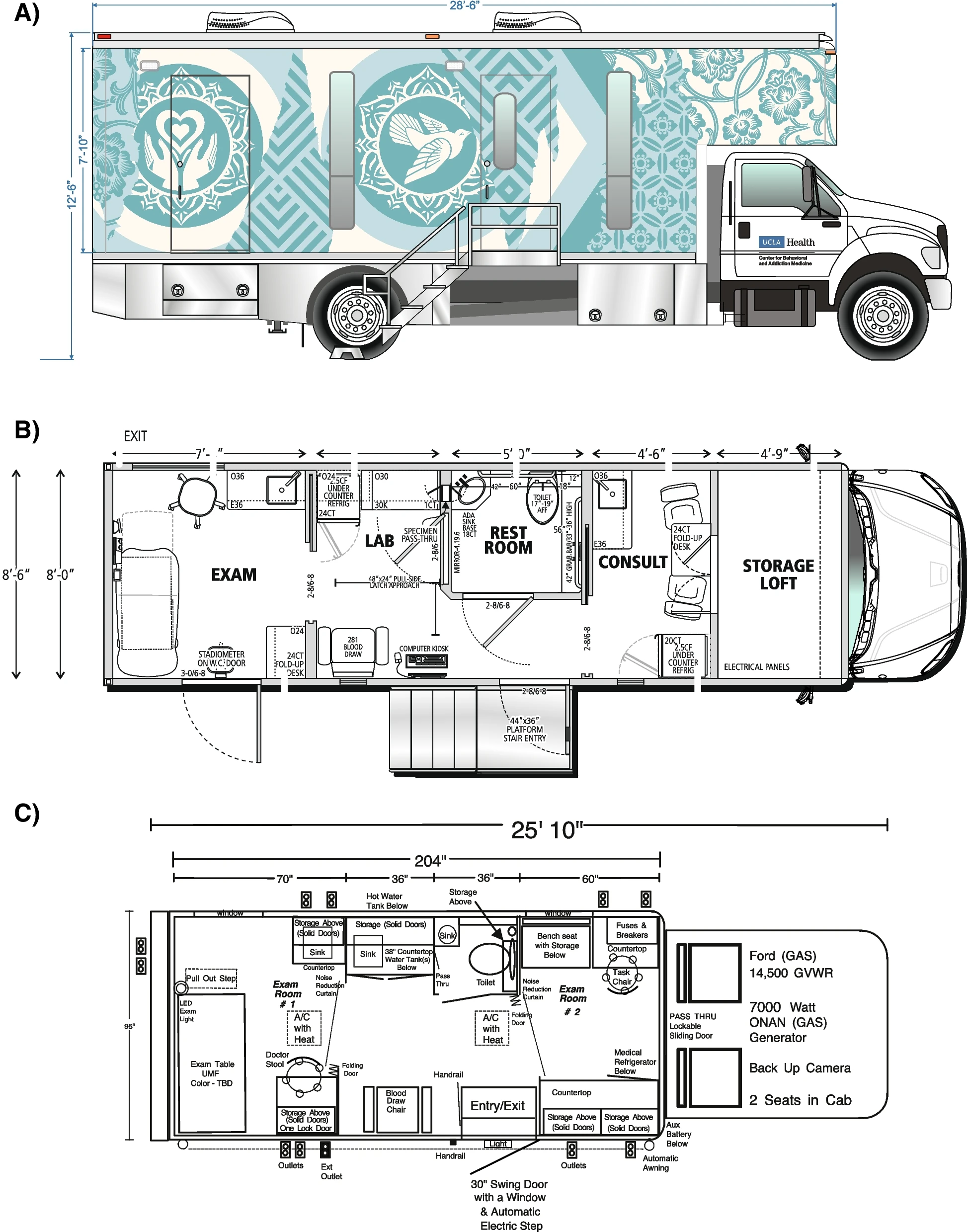
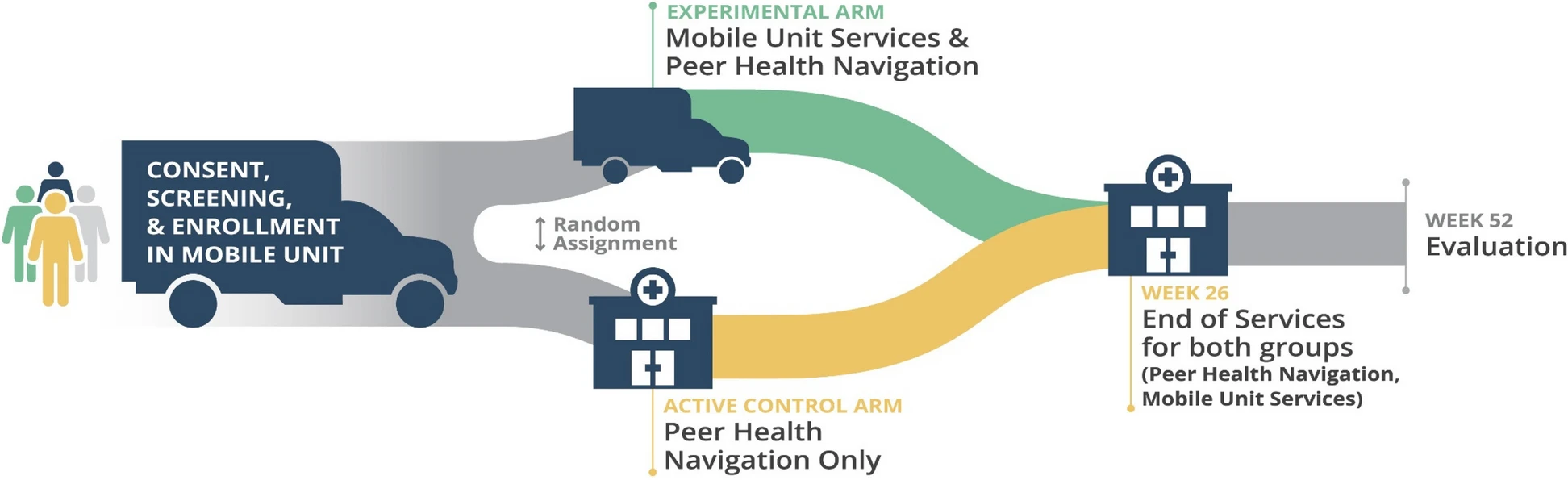
The randomized study of 447 participants was conducted in Houston, Los Angeles, New York, Philadelphia, and Washington, D.C. Eligible participants were randomized to either an intervention or active control arm. Intervention arm participants received “one-stop” health services in a mobile health unit and peer navigation from a peer recovery coach for 26 weeks. During this time, the mobile unit provided participants with primary care services, including MOUD, ART, PrEP, sexually transmitted infection and harm reduction services, as well as screening and referral for hepatitis, mental health issues, and other medical conditions. After 26 weeks, participants in the intervention arm were referred to health services available in the community. Active control arm participants received peer navigation to similar health services available in the community throughout the trial.
“Although not statistically significant, a key finding of the study was that the study group who received care through mobile medical units plus peer navigation had 70 percent lower odds for all-cause mortality (three deaths out of 224 participants) compared to the control arm receiving peer navigation to local services alone (10 deaths out of 223 participants),” said Dr. Myron Cohen, HPTN co-principal investigator, and director of the Institute for Global Health at the University of North Carolina in Chapel Hill. “More research is needed to confirm the study results and examine the long-term effects of mobile healthcare units, including their cost-effectiveness and ability to improve health outcomes.”

