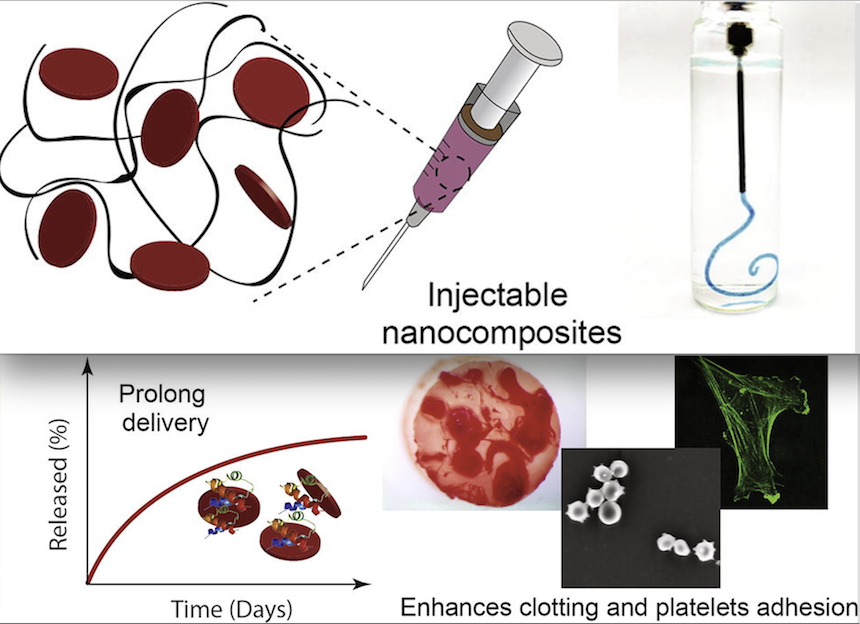
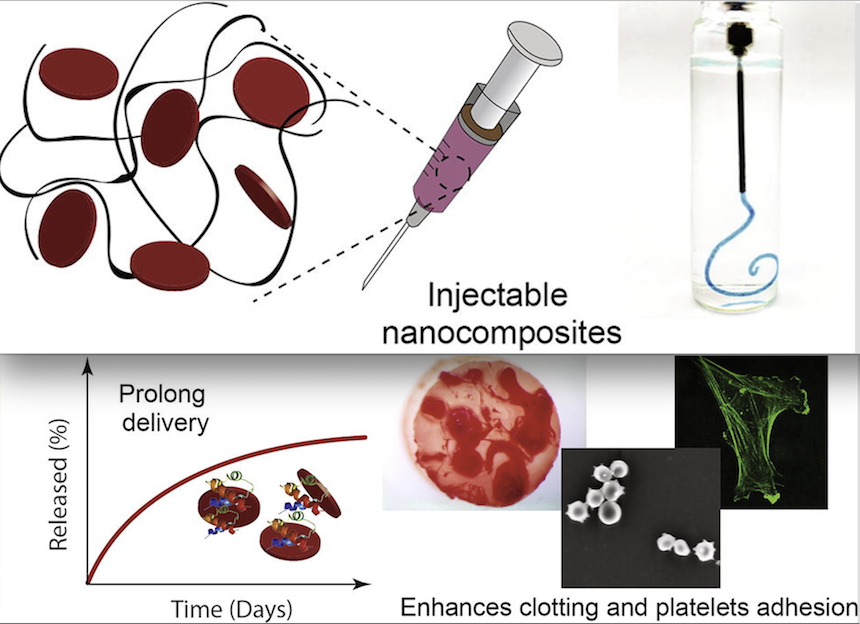
With a gelling agent commonly used in preparing pastries, researchers from the Inspired Nanomaterials and Tissue Engineering Laboratory have successfully fabricated an injectable bandage to stop bleeding and promote wound healing.
In a recent article “Nanoengineered Injectable Hydrogels for Wound Healing Application” published in Acta Biomaterialia, Dr. Akhilesh K. Gaharwar, assistant professor in the Department of Biomedical Engineering at Texas A&M University, uses kappa-carrageenan and nanosilicates to form injectable hydrogels to promote hemostasis (the process to stop bleeding) and facilitate wound healing via a controlled release of therapeutics.
“Injectable hydrogels are promising materials for achieving hemostasis in case of internal injuries and bleeding, as these biomaterials can be introduced into a wound site using minimally invasive approaches,” said Gaharwar. “An ideal injectable bandage should solidify after injection in the wound area and promote a natural clotting cascade. In addition, the injectable bandage should initiate wound healing response after achieving hemostasis.”
The study uses a commonly used thickening agent known as kappa-carrageenan, obtained from seaweed, to design injectable hydrogels. Hydrogels are a 3-D water swollen polymer network, similar to Jell-O, simulating the structure of human tissues.
When kappa-carrageenan is mixed with clay-based nanoparticles, injectable gelatin is obtained. The charged characteristics of clay-based nanoparticles provide hemostatic ability to the hydrogels. Specifically, plasma protein and platelets form blood adsorption on the gel surface and trigger a blood clotting cascade.
“Interestingly, we also found that these injectable bandages can show a prolonged release of therapeutics that can be used to heal the wound” said Giriraj Lokhande, a graduate student in Gaharwar’s lab and first author of the paper. “The negative surface charge of nanoparticles enabled electrostatic interactions with therapeutics thus resulting in the slow release of therapeutics.”

