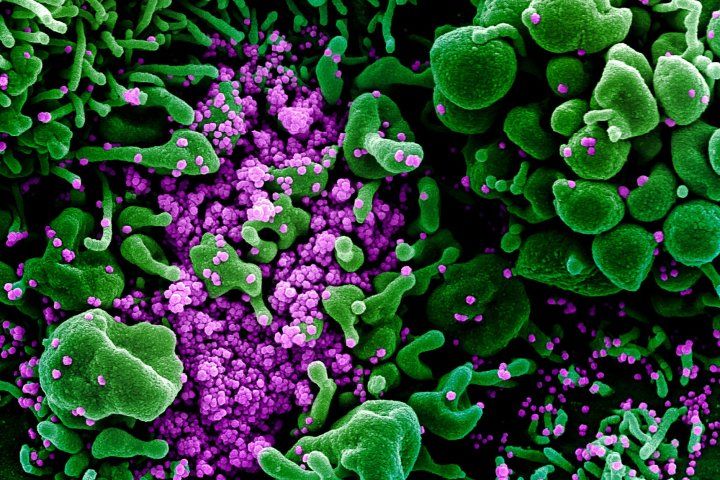
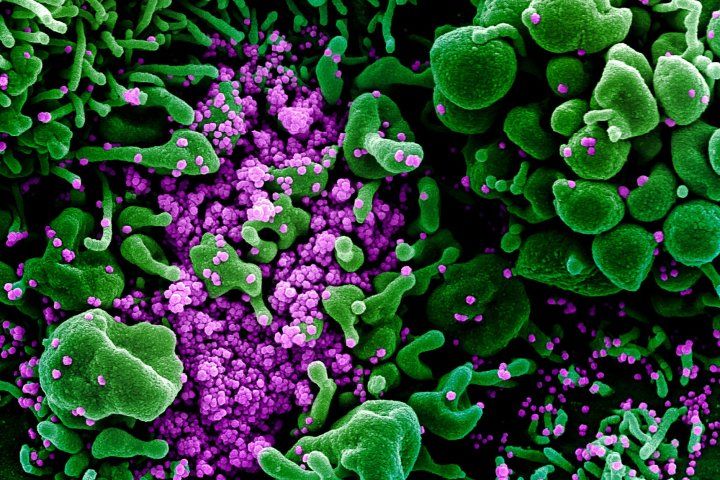
Researchers from UC San Francisco and the Chan Zuckerberg Biohub (CZ Biohub) have developed a new approach for COVID-19 testing that detects a distinct pattern of immune gene expression in infected individuals. This type of test could be used as a check against possible errors generated by the standard tests that directly detect the SARS-CoV-2 virus, the scientists said.
In addition, the gene expression patterns seen in COVID-19 patients in the study indicate that, unlike other respiratory viruses, SARS-CoV-2 may suppress immune reactions in the early stages of infection, setting the stage for the virus to spread before patients develop symptoms.
The immune response to respiratory infections is largely responsible for symptoms like fever, nasal congestion and cough, which might typically encourage someone to isolate and seek testing. Because people with COVID-19 are most infectious early in their disease course, this suppressed immune response in COVID’s first stages makes it more likely that individuals will infect others before they realize they are sick.
The leaders of the new study, published online in Nature Communications on November 17, 2020, say that although the new testing approach analyzes completely different molecules — from the person infected, rather than from the virus that infects the person — it can be implemented using the same PCR technology on the same nasal swab samples. It could be used as a standalone test, or even combined into the same testing panels used in standard PCR tests to detect the virus. Combining the technologies could lessen the chances of false negative or false positive results, the researchers said.
“Without even having to detect the virus itself, these tests to measure changes in the expression of immune-related genes can determine whether or not someone has COVID-19,” said co-senior study author Chaz Langelier, MD, PhD, assistant professor in the Division of Infectious Diseases in the UCSF Department of Medicine, who led the research with Amy Kistler, PhD, of CZ Biohub.
The UCSF scientists created three proof-of-concept versions of the new test — one based on readouts of gene activity from three key genes, one based on readouts from 10 genes, and one based on 27 genes. The tests independently detected COVID-19 infection in clinically confirmed cases, increasing in sensitivity with the number of genes included.
Langelier envisions using one of these measures of gene activation both to flag false negative viral PCR tests, in which direct viral detection fails, and to rule out false positive results, which may arise from cross-contamination between samples in testing labs. False positives become an increasing challenge when performing routine testing of people without symptoms in populations with relatively few cases. Even adding just a few genes to the currently used virus-detecting tests could greatly improve accuracy, he said.
To determine which changes in gene activity were distinctive to SARS-CoV-2 infection the researchers first surveyed all the genetic material in swab samples from the upper respiratory tract, so that they could identify the most important and predictive indicators.
“We used a ‘metagenomic’ approach — from each sample we sequenced all the genetic information, both from the patient and from any microbes present,” said Eran Mick, PhD, bioinformatics scientist at UCSF and CZ Biohub, a first author of the study along with the Biohub’s Jack Kamm, PhD. “We looked both at the microorganisms and at human gene expression, as measured by levels of RNA that has been transcribed from switched-on genes.”
The researchers examined samples from patients with respiratory symptoms who were tested for COVID-19 as a possible explanation of their illness. The tests showed many of the patients did have COVID-19, but some of them turned out to be infected with more common respiratory viruses (like the flu) or to be suffering from nonviral conditions.
“In samples from COVID-19 patients we initially expected to find a large activation of genes that drive pro-inflammatory pathways, given how horrible we know this virus can be,” Mick said. “We were surprised that it turned out to be the opposite. Some inflammatory pathways that were activated by other viruses were not in fact activated in COVID-19.”
With computer algorithms and a great deal of number crunching, the UCSF scientists were able to identify a distinct pattern of gene expression associated with a tamping down of specific immune responses that occurs early during SARS-CoV-2 infection. The changes differed from those seen in other viral respiratory infections or nonviral respiratory illnesses, allowing for a specific diagnosis of COVID-19.
The pattern of immunosuppressive gene expression the researchers identified in COVID-19 may explain the stealthy nature of this highly transmissible virus, the researchers said. Unlike the first SARS-CoV virus, which caused global concern and killed hundreds in 2002 and 2003, SARS-CoV-2 appears to be most transmissible before the onset of symptoms, or just as symptoms first arise, making it more likely that individuals will infect others before they realize they are sick.
“We have concluded from our work that there is an immunosuppressive effect taking place that prevents symptoms from developing early during infection despite high levels of viral replication,” Langelier said. “It’s a brilliant strategy, if you’re a virus.”
However, as is now well known, in a subset of COVID-19 patients, after the virus makes its way down the respiratory tract and infects cells within the lungs, the immune system eventually launches an overly aggressive response that damages the patient’s own tissues. Intensive-care treatment aims to counter this often-deadly immune reaction, but that does not mean early immunosuppressive treatment would result in better outcomes.
“Our findings of a diminished inflammatory response by the innate immune system suggest that treatments that suppress the immune system early during COVID-19 infection are unlikely to be beneficial,” Langelier said. “The medical community already knows from the RECOVERY study that the immunosuppressive steroid drug dexamethasone benefits patients with severe disease, but for those with mild disease there was a trend toward worse outcomes with treatment.”
The Nature Communications study was based on analysis of one early time point during the course of infection, and patient outcomes were unknown. But the UCSF researchers also are participating in the multicenter, prospective, observational COMET study of patients hospitalized with COVID-19, in which samples are collected throughout the course of the disease, and clinical progression and disease outcomes are tracked.
It may be that changing patterns of gene activation affecting the immune system could help predict which individuals are most likely to experience severe illness as a result of COVID-19 infection. The research might also lead to the identification of new targets for treatment and new therapeutic strategies.
“Especially with the multiple approaches being taken by the many researchers who are participating in the nationwide study, I think it’s possible that we may find predictors of severe disease that are clinically actionable,” Langelier said.

