The most frequently performed imaging exam in medicine “the chest X-ray” holds ‘hidden’ prognostic information that can be harvested with artificial intelligence (AI), according to a study by scientists at Massachusetts General Hospital (MGH). The findings of this study, published in JAMA Network Open, could help to identify patients most likely to benefit from screening and preventive medicine for heart disease, lung cancer and other conditions.
AI technology automates many aspects of our daily lives, such as your smartphone’s speech-recognition function, photo tagging on social media, and self-driving cars. AI is also responsible for major advances in medicine; for example, several groups have applied AI to automate diagnosis of chest X-rays for detection of pneumonia and tuberculosis.
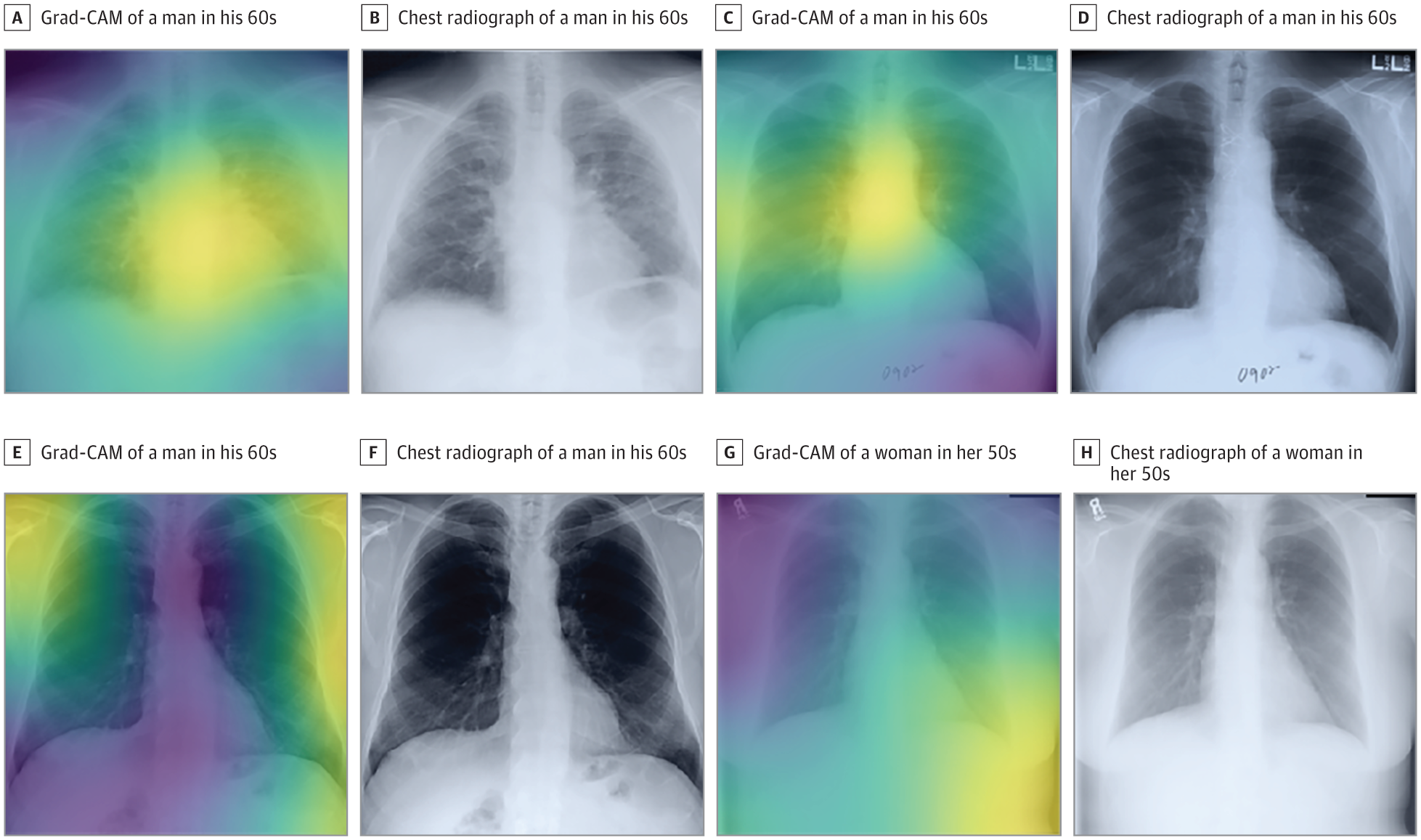
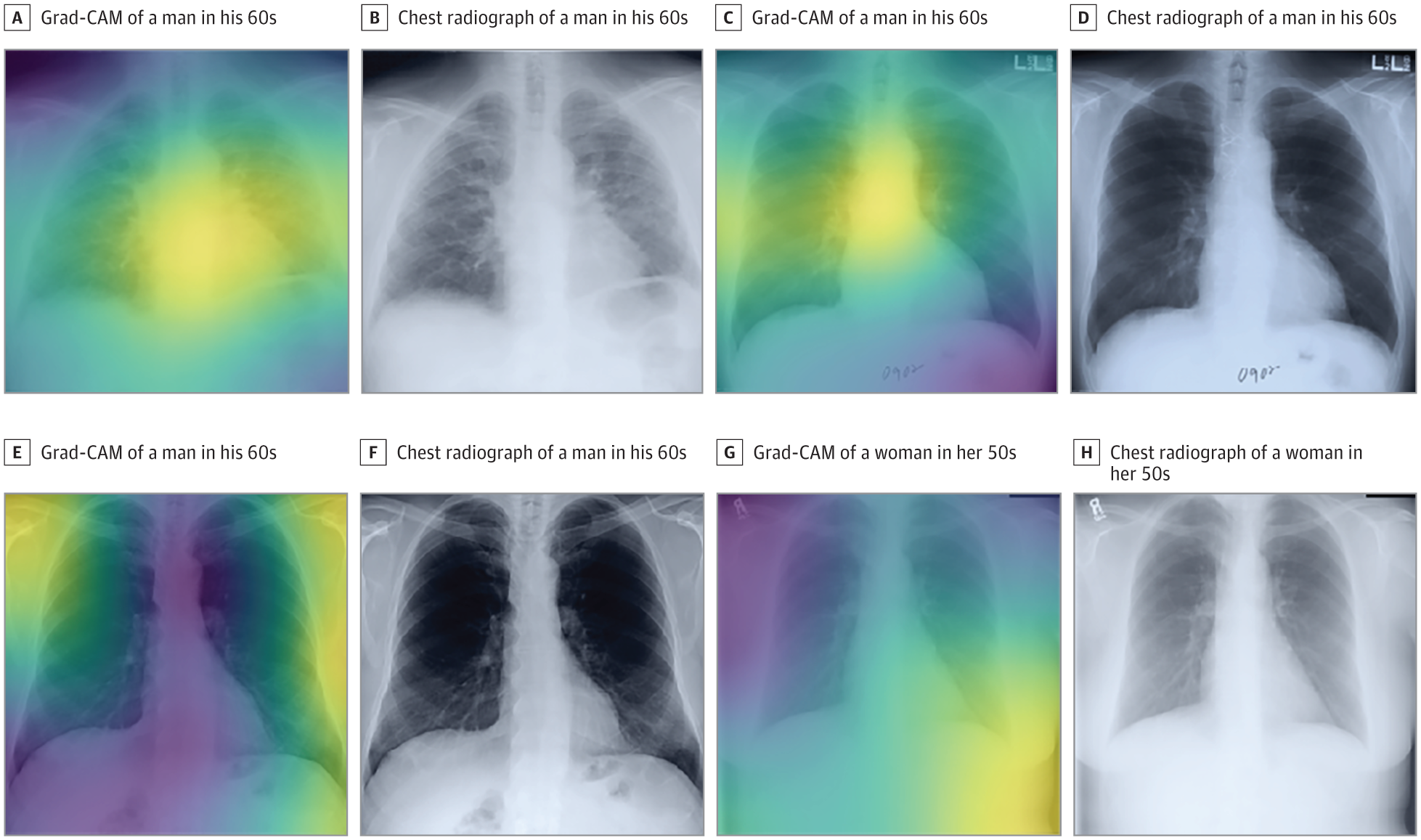
If this technology can make diagnoses, asked radiologist Michael Lu, MD, MPH, could it also identify people at high risk for future heart attack, lung cancer, or death? Lu, who is director of research for the MGH Division of Cardiovascular Imaging and assistant professor of Radiology at Harvard Medical School, and his colleagues developed a convolutional neural network, a state-of-the-art AI tool for analyzing visual information, called CXR-risk. CXR-risk was trained by having the network analyze more than 85,000 chest X-rays from 42,000 subjects who took part in an earlier clinical trial. Each image was paired with a key piece of data: Did the person die over a 12-year period? The goal was for CXR-risk to learn the features or combinations of features on a chest X-ray image that best predict health and mortality.
Next, Lu and colleagues tested CXR-risk using chest X-rays for 16,000 patients from two earlier clinical trials. They found that 53% of people the neural network identified as “very high risk” died over 12 years, compared to fewer than 4% of those that CXR-risk labeled as “very low risk.” The study found that CXR-risk provided information that predicts long-term mortality, independent of radiologists’ readings of the x-rays and other factors, such as age and smoking status.
Lu believes this new tool will be even more accurate when combined with other risk factors, such as genetics and smoking status. Early identification of at-risk patients could get more into preventive and treatment programs. “This is a new way to extract prognostic information from everyday diagnostic tests,” says Lu. “It’s information that’s already there that we’re not using, that could improve people’s health.”

