With 1.2 million deaths in the 2020, or 23% of the total number of deaths, cancer is the second biggest killer in the European Union.
The figure is all the more tragic given 40% of these cancers could be prevented through early detection and lifestyle change such as not smoking or regular exercise.
Research on the future of medicine offers hope, however, with significant progress forecast in the prevention and treatment of the disease in the decades to come. The rise of Artificial Intelligence (AI), among others, is one of the significant causes for optimism.
What exactly does AI in healthcare involve?
Many recent research articles show that AI has the potential to transform healthcare by offering new ways to improve the prevention, diagnosis, treatment and management of cancer across many therapeutic areas – oncology, cardiology, and ophthalmology in particular- and across the value chain, from research, development, production down to marketing. Overall, patients stand to enjoy much better care.
Glancing over market figures, the growth of AI in healthcare is evident from the large number of players. Leaving aside the flourish of AI startups, 18 out of the 47 multinationals providing AI currently offer healthcare solutions. Out of these, 80% offer innovative solutions related strictly to treatment, while 20% produce efficiency-based tools to optimise resources and hone healthcare technology.
AI is set to contribute to six areas in particular:
- Medical research: AI can accelerate the development of new treatments by analysing large bulks of data to identify promising chemical compounds and predict their efficacy. The technology is set to have a major impact on drug development, speeding up clinical research by identifying patients who are eligible for clinical trials and analysing data generated by these trials
- Medical diagnosis: AI can help doctors make faster and more accurate diagnoses by analysing medical data (X-ray images, lab results, specific medical histories, for example). AI algorithms can detect early signs of disease and help identify the most appropriate treatment. Among many other examples, the Wisconsin Breast Cancer used a specific machine learning algorithm which was successfully applied to diagnose breast cancer and achieved 98.53% classification accuracy.
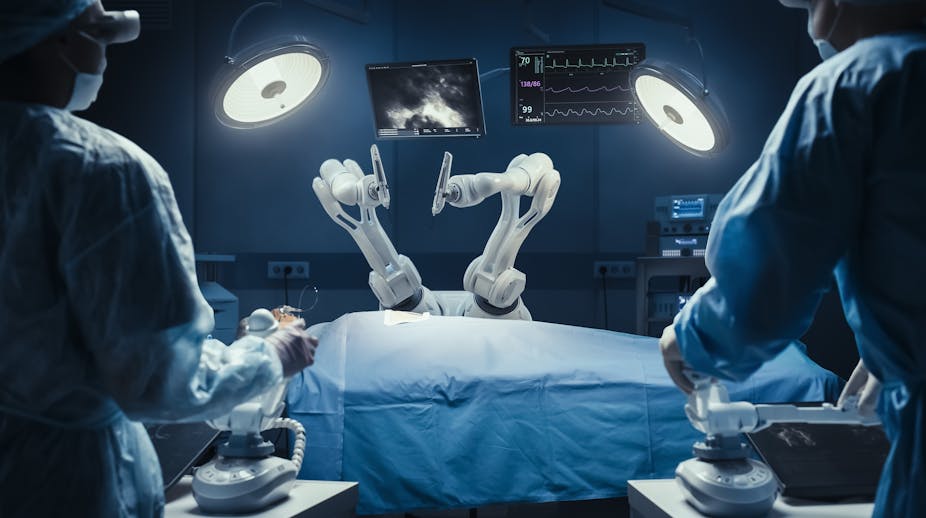
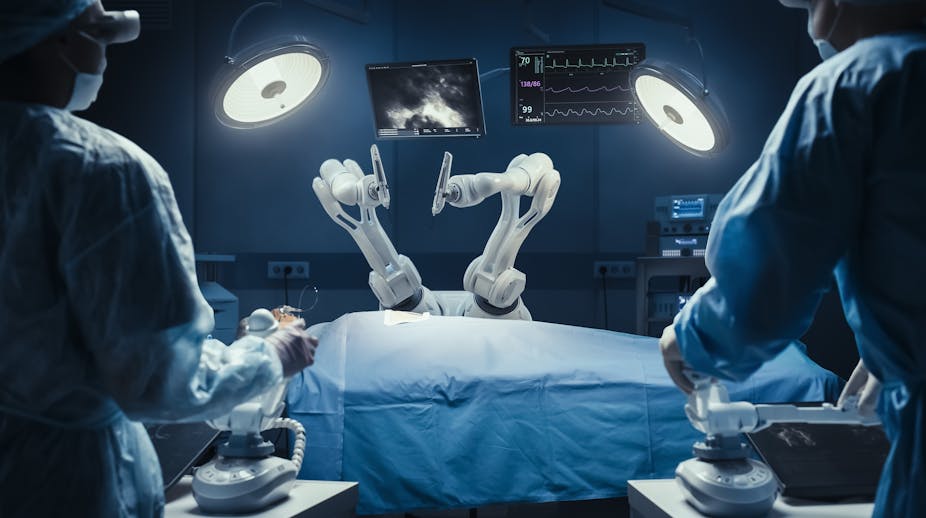
- Surgery assistance: AI can help surgeons plan and perform complex surgical procedures, including preoperative planning, intra-operative approaches, and prediction of postoperative complications. AI-assisted surgical robots allow for greater precision and quicker post-operative recovery for patients.
- Patient monitoring: AI can be used to monitor patients’ vital signs, including heart rate, blood pressure or blood sugar level, and alert healthcare professionals in the event of abnormalities. This is predicted to be game-changing for patients with chronic diseases, enabling thorough monitoring and early intervention should they experience complications.
- Personalised treatment: AI can take into consideration vast amounts of medical data to determine the most targeted treatment for patients, factoring in their genetic profile, medical history, lifestyle and a host of other specific traits.
- Medical record management: AI can automate electronic medical record management, thereby making medical record management more efficient and accurate while ensuring the confidentiality and security of patient information.
Diagnostic announcement procedure
Out of the areas outlined above, the market for AI-assisted medical diagnosis is faring particularly well. Worth $1.3 billion today, it is expected to see an annual growth rate of over 23% in the next five years to reach $3.7 billion in 2028. There is already strong demand for cloud-based medical image analysis software in particular. Fields such as mammography, CT-scans or MRIs are set to be among the first to be benefit from the technology.
In practice, however, many hospital centres are grappling with a lack of technological resources, making it difficult for them to tap into AI’s potential. Take the pathology slides on the basis of which biological anomalies are analysed: although all of them should be digitised to train AI models, the vast majority of European institutions currently lack the equipment to do so.
Treatment management, support and post-treatment monitoring
AI can be used at every stage of cancer care, allowing healthcare professionals to focus on high value-added tasks such as direct patient care and psychological support, critical technical decision-making, and clinical trials. This can lead to improved patient outcomes and a more efficient healthcare system.
Three areas stand in particular to benefit from the technology:
- organisational management tools, which save your doctor much time in routine tasks. Some of these might help monitor patient flow, slash the administrative burden, and record notes thanks to automated transcription software to complete medical records.
–predictive analytic tools, which mine and analyse large quantities of patient data and determine which health categories a patient belongs to. This allows for a more personalised and efficient treatment.
- AI-powered surgical assistance tools, based on medical robotics. These technologies are still too often used for simple surgical procedures, such as stitching.
- Remote monitoring allows medical professionals to use digital medical devices to remotely interpret patients’ health data collected in their homes and make decisions about their care. Remote monitoring systems aim to improve patients’ health through regular monitoring.
- Chatbots can also be included in a wide range of applications (Messenger, Slack). They can be utilised throughout the patient care pathway, but are especially helpful during the monitoring period, in which continued support is crucial.
The limits of AI in healthcare
For all those exciting prospects, we will nevertheless need to overcome a set of challenges before we can enjoy the full range of benefits of AI-assisted healthcare.
For one, AI has yet to become more sophisticated from a technical viewpoint. For example, the current absence of a universal format for data health makes it tricky to clean it up and transfer it from one software or computer to the next. The vast majority of AI solutions also require to be trained by humans – and not any humans. In collaboration with healthcare professionals, engineers will need to carefully listen to the medical community’s needs and reflect them in emerging AI.
It’s no secret sociocultural and ethical questions will also need to be taken into consideration. Data protection remains a real issue for many citizens even though the European Union’s 2018 framework regulation for processing data, the General Data Protection Regulation (GDPR), has handed more power to individuals to dictate how companies handle their personal information. The EU AI Act, the world’s first comprehensive legislation to regulate AI machines posing risks to health, human rights and safety, should also go some way in alleviating those concerns.
This article was co-written with Prof. Frédéric Jallat’s former student, Rym Aouchiche, who currently works as a Life Sciences & Strategy Associate Consultant at IQVIA.![]()
![]()
Frédéric Jallat, PhD, Professeur de marketing à ESCP Business School, professeur vacataire, ESCP Business School
This article is republished from The Conversation under a Creative Commons license.

