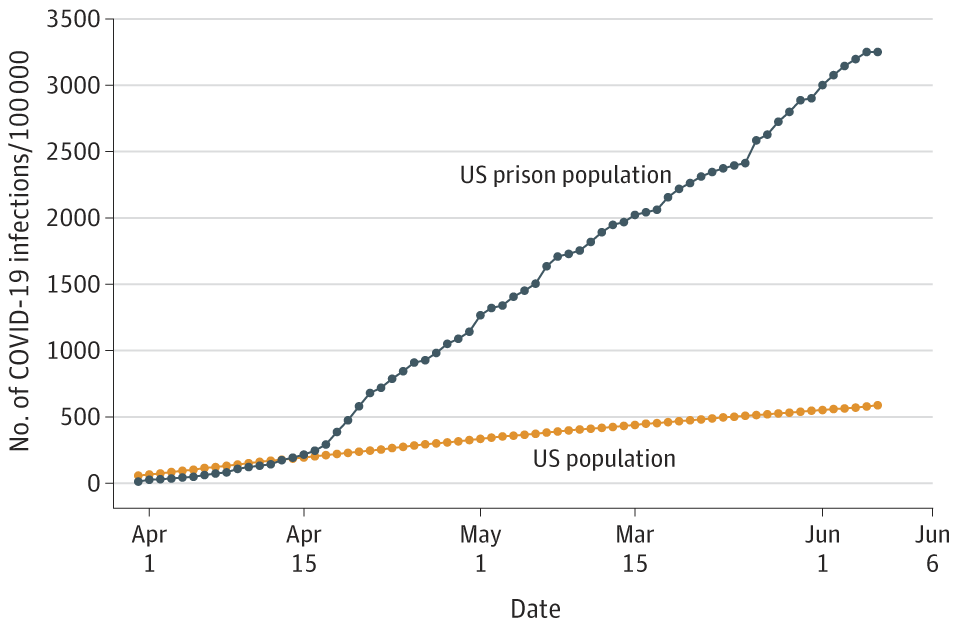
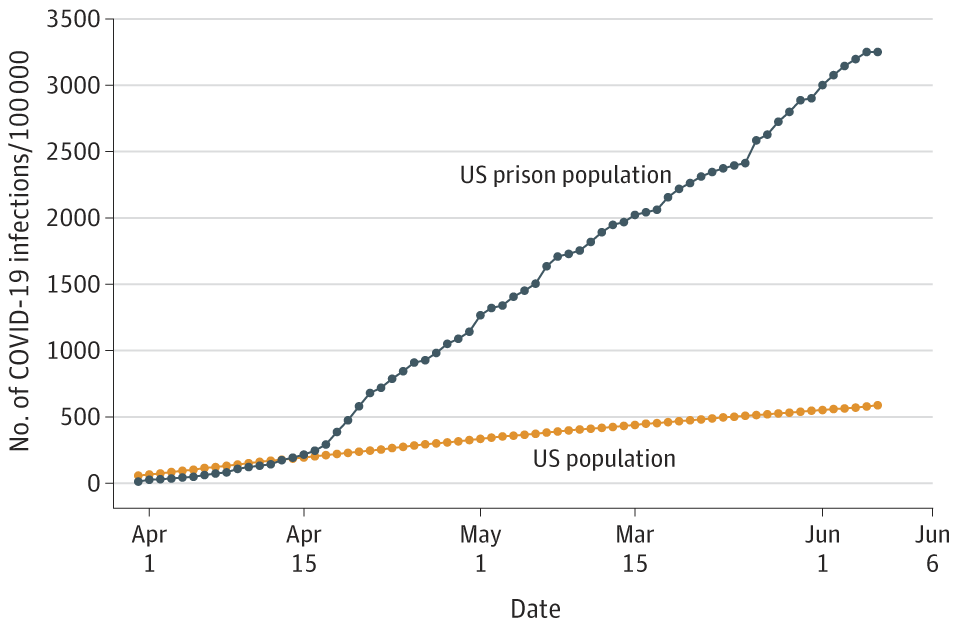
A new analysis led by researchers at Johns Hopkins Bloomberg School of Public Health found that the number of U.S. prison residents who tested positive for COVID-19 was 5.5 times higher than the general U.S. population, with a prisoner case rate of 3,251 per 100,000 residents as compared to 587 cases per 100,000 in the general population.
The researchers also found the death rate of U.S. prisoners was 39 deaths per 100,000 prison residents, higher than that of the U.S. population at 29 deaths per 100,000 people. After adjusting for age and sex differences between the two groups, the death rate would be three times higher for prisoners compared to the general U.S. population.
The findings were published online in a research letter in JAMA.
The study, which analyzed cases and deaths from March 31 to June 6, 2020, found that COVID-19 cases in prisons increased by 8.3 percent per day compared to 3.4 percent in the general population. The analysis includes COVID-19 cases among prisoners, including active confirmed cases, recoveries, and decedents, posted on publicly available data sources such as correction departments’ websites, news reports, and press releases.
“While these numbers are striking, we actually think the disparities within prisons is much greater,” says lead author Brendan Saloner, PhD, associate professor in the Department of Health Policy and Management at the Bloomberg School. “Some prisons are not reporting any cases, others are not even testing inmates, so the need for policies to protect incarcerated populations is more important than ever.”
For the study, the Bloomberg School researchers collaborated with the UCLA Law COVID-19 Behind Bars Data Project, a new initiative based at the University of California, Los Angeles–led by senior author, Sharon Dolovich, JD, PhD, at the University of California, Los Angeles School of Law–that collects data on prisoners in state and federal prisons.
For their analysis of COVID-19 deaths, the researchers drew from information available from departments of corrections and external medical examiner reports. Using data from the Centers for Disease Control and Prevention and the U.S. Census Bureau’s American Community Survey, the researchers were able to gather state-level data about COVID-19 cases, deaths, and demographics for the general U.S. population.
The researchers counted COVID-19 cases and deaths separately for prisoners and the general population. During the study period, there were 42,107 cases of COVID-19 and 510 deaths among 1,295,285 prison residents. Among the U.S. population, there were 1,920,904 infections and 95,608 deaths.
Prison populations are especially vulnerable to the spread of a highly infectious disease like COVID-19. Close confinement, limited access to personal protective equipment, and high rates of preexisting respiratory and cardiac conditions are factors that can exacerbate the spread of COVID-19 among the two-plus million people incarcerated in America’s jails, prisons, and correctional facilities. Policies that have potential to curb the spread of disease include the early release of prisoners unlikely to pose a risk of reoffending, implementing strong infection control practices, and using widespread testing.
“Prisoners have a right to adequate protection of their health while incarcerated,” says Saloner. “The reality of these findings shows that we aren’t coming anywhere close to meeting their basic needs. Ultimately, it creates a dangerous situation for the inmates, prison staff, the communities that prisons are located in, and in our overall effort to contain the crisis.”

