As the biggest vaccination effort in U.S. history gets underway, several states may not have a sufficient number of facilities in some areas to administer the COVID-19 vaccine to all residents who want it, according to a new analysis from the University of Pittsburgh School of Pharmacy and the nonprofit West Health Policy Center.
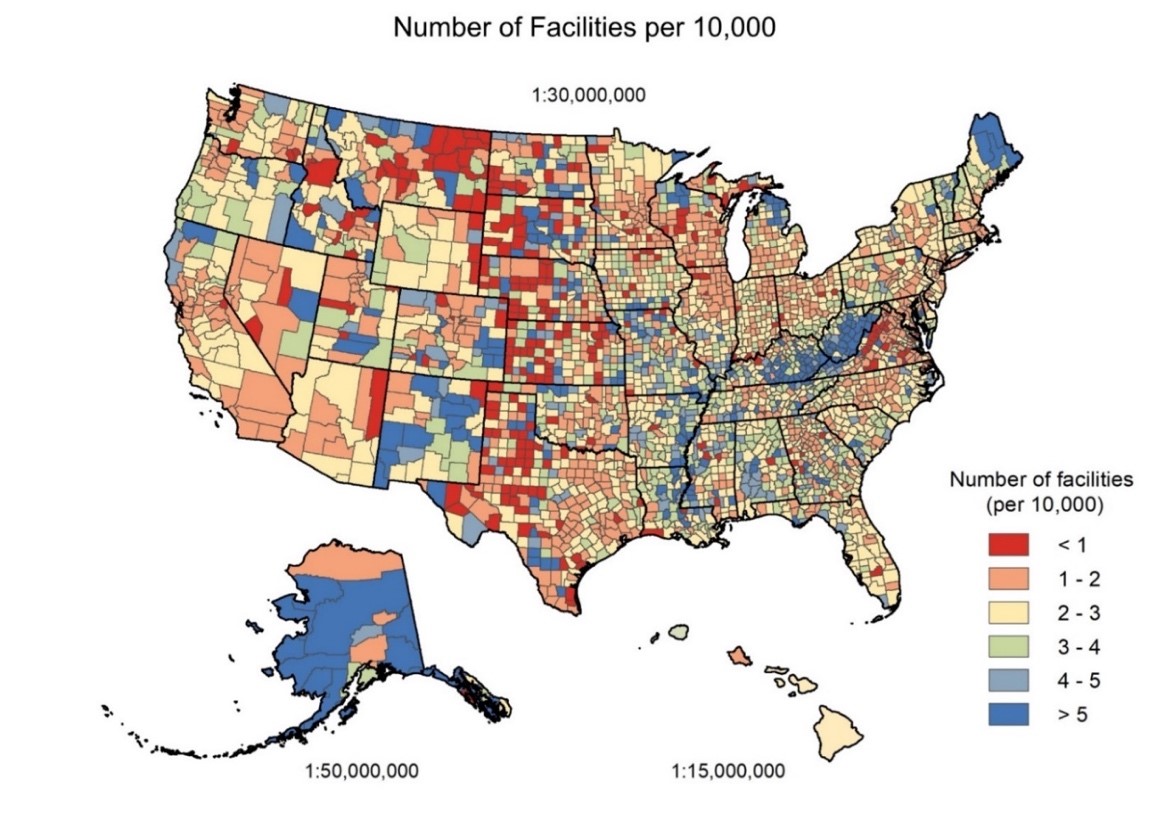
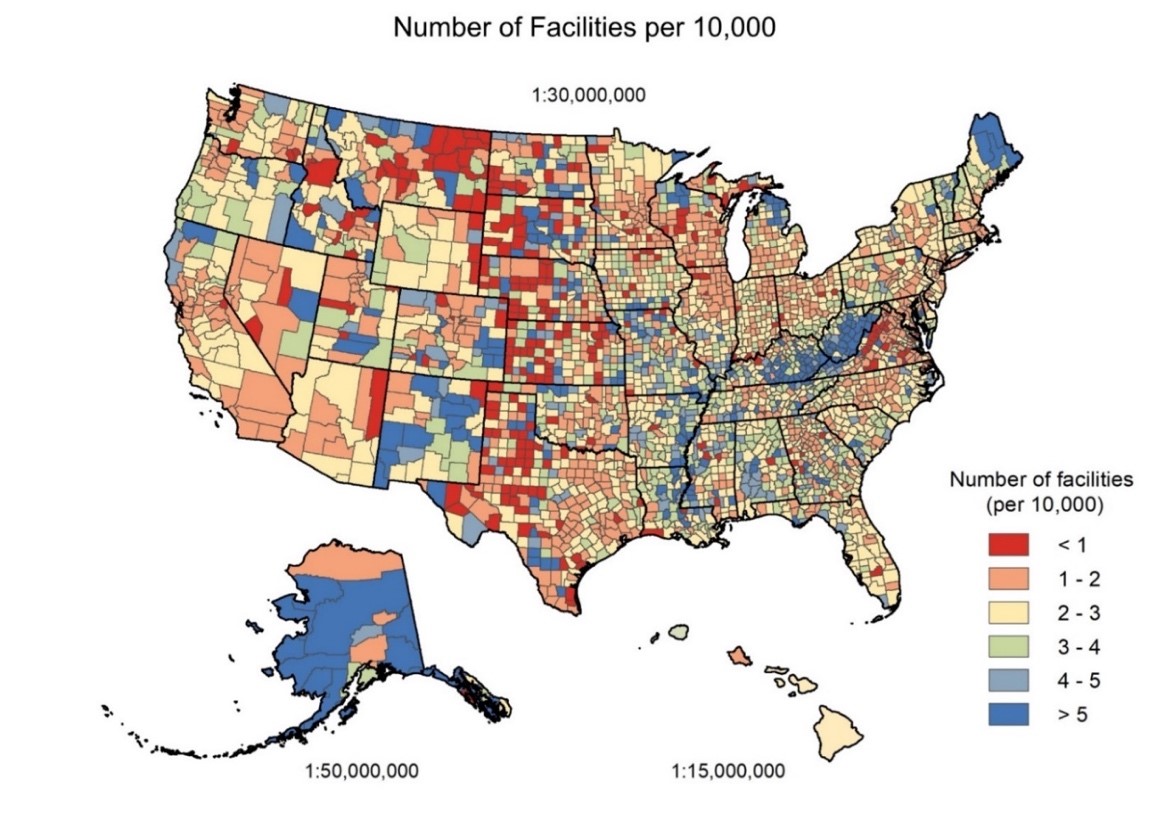
In what is believed to be the first county-level analysis of the nation’s potential COVID-19 vaccine facilities, which include community pharmacies, federally qualified health centers, hospital outpatient departments and rural health clinics, the researchers found that more than a third (35%) of U.S. counties have two or fewer of these facilities and nearly 1 in 10 counties have fewer than one facility per 10,000 residents.
The analysis, including an interactive, open-access map, titled VaxMap, and white paper, was published online today by West Health.
“The U.S. has large geographic variation in population access to potential COVID-19 vaccine administration facilities, particularly at the county level,” said Inmaculada Hernandez, Pharm.D., Ph.D., Assistant Professor at the Pitt School of Pharmacy and senior author of the study.
“This highlights the need for state and local public health officials to tailor their vaccine distribution and administration plans to their specific populations and the current limitations of their state’s existing healthcare infrastructure,” said Lucas Berenbrok, Pharm.D., Assistant Professor at the Pitt School of Pharmacy and first author of the study.
Researchers used geographic information system (GIS) software to map more than 70,000 potential COVID-19 vaccine administration facilities and calculate the average driving distance to the closest facility for simulated citizens, including high-risk populations such as people age 65 or older.
The counties with the fewest vaccination facilities relative to the size of their populations are located in Texas, Kansas, Nebraska, Montana and Virginia. When it comes to driving distance, residents of North Dakota, South Dakota, Montana, Wyoming, Nebraska, and Kansas face the longest drives, with over 10% living more than 10 miles away from the closest facility.
For older adults it’s even worse. In 12% of counties, at least half of the older population have a more than 10-mile drive. In North and South Dakota, 25% of older adults are more than 10 miles away from a facility.
“We did the analysis to help states and counties throughout the U.S. identify potential problem areas for vaccine administration and enact effective strategies and take measures to overcome them,” said Tim Lash, President of the West Health Policy Center. “Clearly there are certain spots throughout the country that need more help and support than others.”
The researchers suggest that state and local authorities in areas with short driving distances and low facility density may consider adding mass vaccination clinics to increase capacity and reduce the time to vaccinate. Conversely, areas with high driving distances may benefit from mobile vaccination clinics to reduce travel-related barriers, and vaccines that require only one dose instead of two may be more effective in ensuring sufficient vaccine uptake.
“Facility density and distance metrics can guide state officials not only in identifying the most appropriate strategy to increase capacity and convenience in each locality, but also in vaccine selection,” said paper co-author Sean Dickson, Director of Health Policy, West Health Policy Center. “When large populations are served by only a few vaccine administration points, additional support to store and dispense vaccine will be needed.”

