When SARS-CoV-2, the virus that causes COVID-19, infects a human cell, it quickly begins to replicate by seizing the cell’s existing metabolic machinery. The infected cells churn out thousands of viral genomes and proteins while halting the production of their own resources. Researchers from Brigham and Women’s Hospital, Massachusetts General Hospital (MGH), and the Broad Institute, studying cultured cells shortly after infecting them with the virus, now have more insight into the metabolic pathways co-opted by the virus. The findings, published in Nature Communications, highlight the potential therapeutic benefit of drugs such as methotrexate, which inhibit folate and one-carbon metabolic pathways appropriated by the virus.
“One of the things we’re lacking in this pandemic is a pill that can be taken orally, as a prophylactic agent, before someone is hospitalized or even before they’re infected,” said corresponding author Benjamin Gewurz, MD, PhD, of the Division of Infectious Diseases. “Monoclonal antibodies have a lot of promise but need to be given intravenously. Blocking the metabolism pathways that viruses rely on to replicate could be a new strategy for treating patients at an early timepoint.”
To identify which metabolic pathways to target, the researchers obtained samples of the virus and cultivated them in a highly protected facility called a BSL-3 laboratory, located at the Broad Institute. They then paired up with the laboratory of co-senior author Vamsi Mootha, MD, of MGH, to apply mass spectrometry approaches to identify the resources being consumed and produced by healthy cells and infected cells. They studied the infected cells at an “eclipse point,” eight hours after infection, when the virus has begun manufacturing its RNA and proteins but has not yet exerted a serious effect on host cell growth and survival.
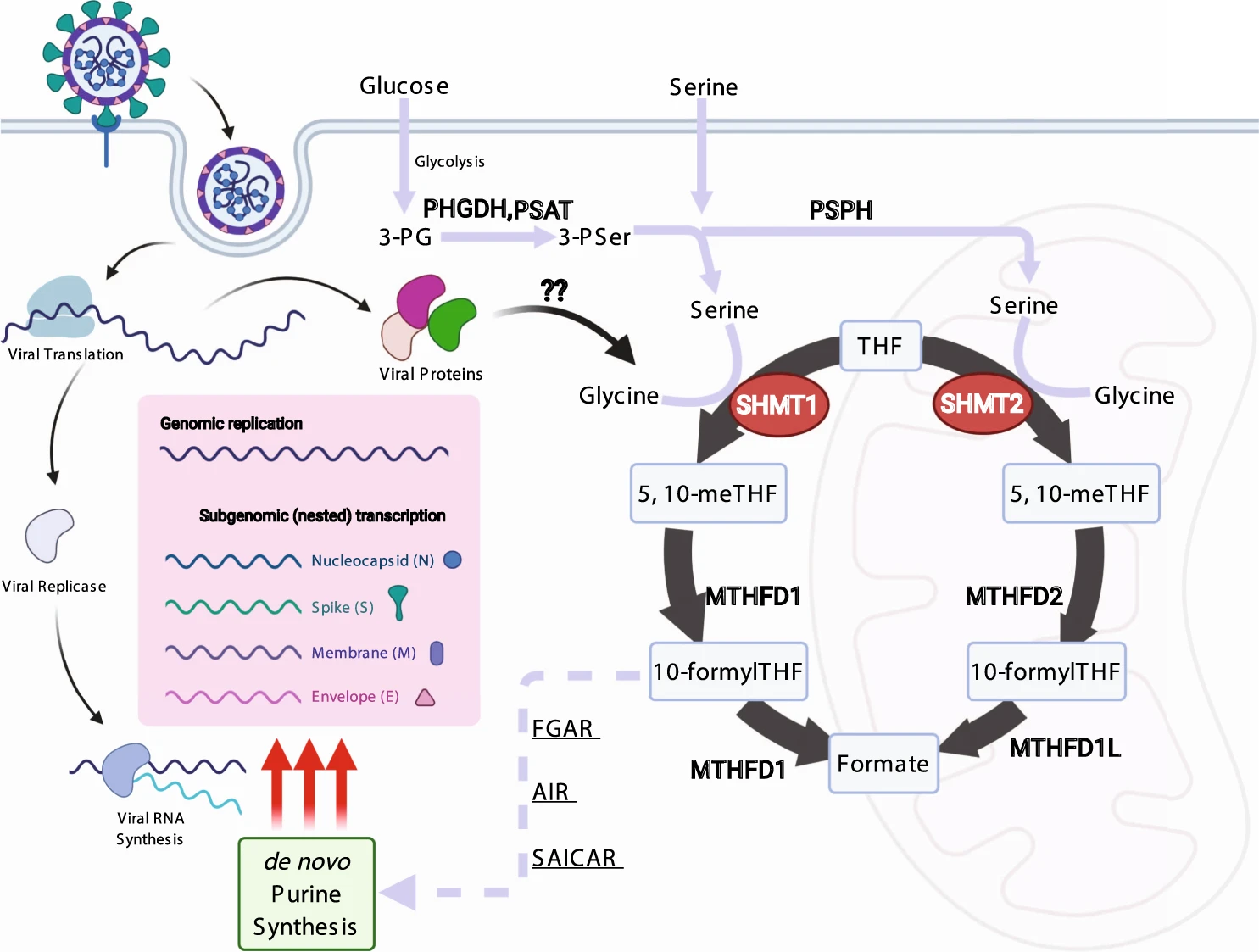
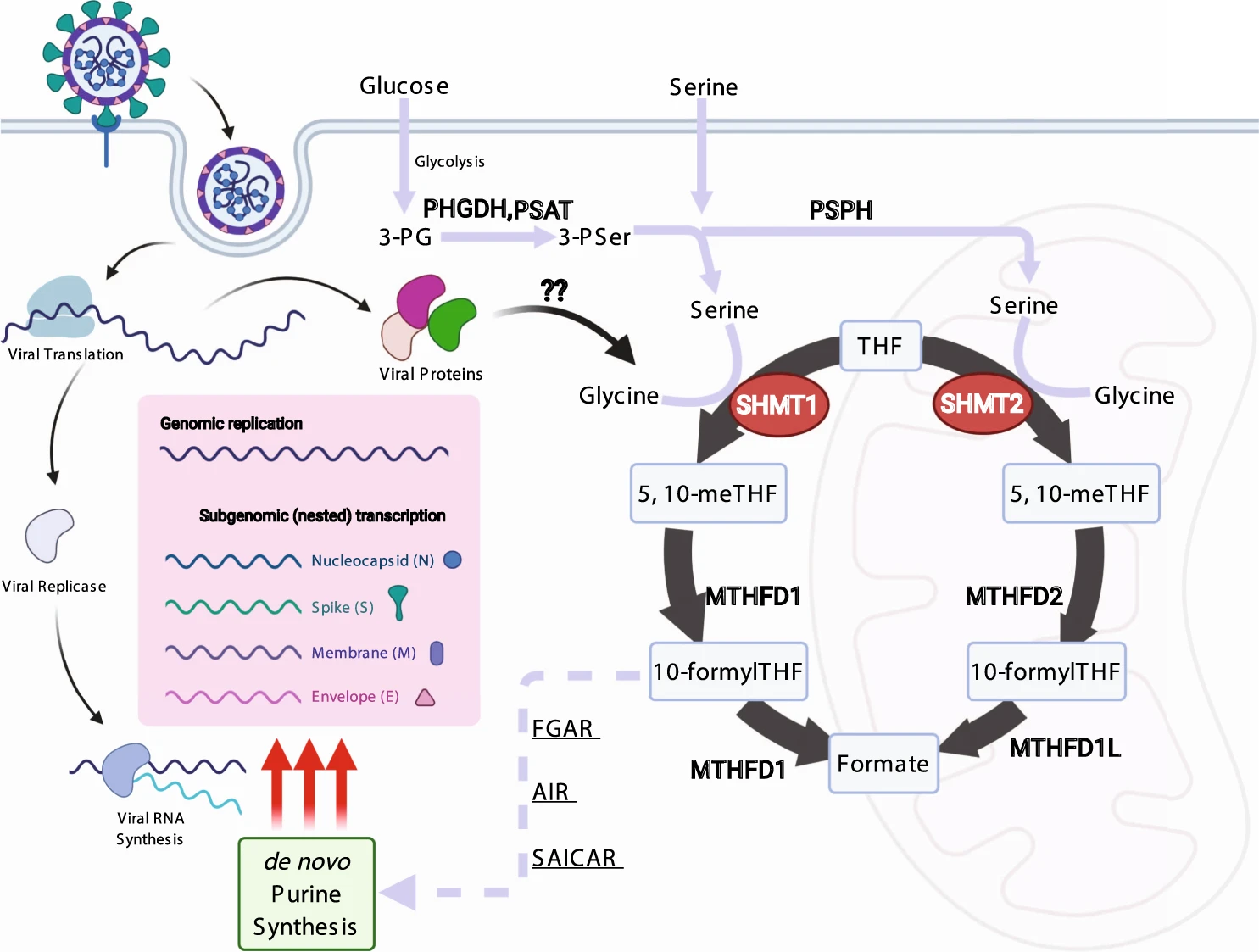
In analyzing the amino acids and thousands of chemical metabolites produced by the cells, the researchers observed that infected cells had depleted stores of glucose and folate. They demonstrated that the SARS-CoV-2 virus diverts building blocks from glucose production to the assembly of purine bases, which are necessary for creating large amounts of viral RNA. Additionally, they found that the 1-carbon pathway used to metabolize folate was hyperactive, thus supplying the virus with more carbon groups for making bases for DNA and RNA.
Drugs that inhibit folate metabolism, like methotrexate, are often used to treat autoimmune conditions like arthritis and could be therapeutic candidates for COVID-19. Methotrexate is currently being assessed as a treatment for the inflammation that accompanies more advanced COVID-19 infections, but the researchers suggest that it could also be beneficial early on. Their study also found that it could offer a synergistic effect when administered with the anti-viral drug remdesivir. Methotrexate’s immune-suppressing properties could make its proper administration as a prophylactic challenging, however. Researchers would need to determine how to maximize the drug’s antiviral effects without significantly compromising a patient’s natural immune response.
Still, Gewurz points out that oral antivirals are an important addition to an arsenal of therapies for COVID-19, serving both as an immediate treatment for infection as well as a defense against new variants and other coronaviruses.
“We’re hoping that, ultimately, we can find a way of preventing viruses from using cells’ metabolism pathways to replicate themselves because that could limit the ability of viruses to evolve resistance,” Gewurz said. “We’re starting to see new viral variants, and we’re hoping that we can stay ahead of that — treating patients before the virus has the chance to make copies of itself that could become resistant to antibodies.”

