A study of all fully vaccinated people in Belgium has assessed the risk factors associated with developing COVID-19 after vaccination. The research, which is being presented at this year’s European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) in Lisbon, Portugal, (23-26 April) and published in the journal Viruses, found that breakthrough infections were more common in those who had received viral vector vaccines than mRNA vaccines. Those who had previously had Covid had a lower risk of breakthrough infections.
More than 80% of adults in Belgium were fully vaccinated (received two doses) by August 11, 2021.
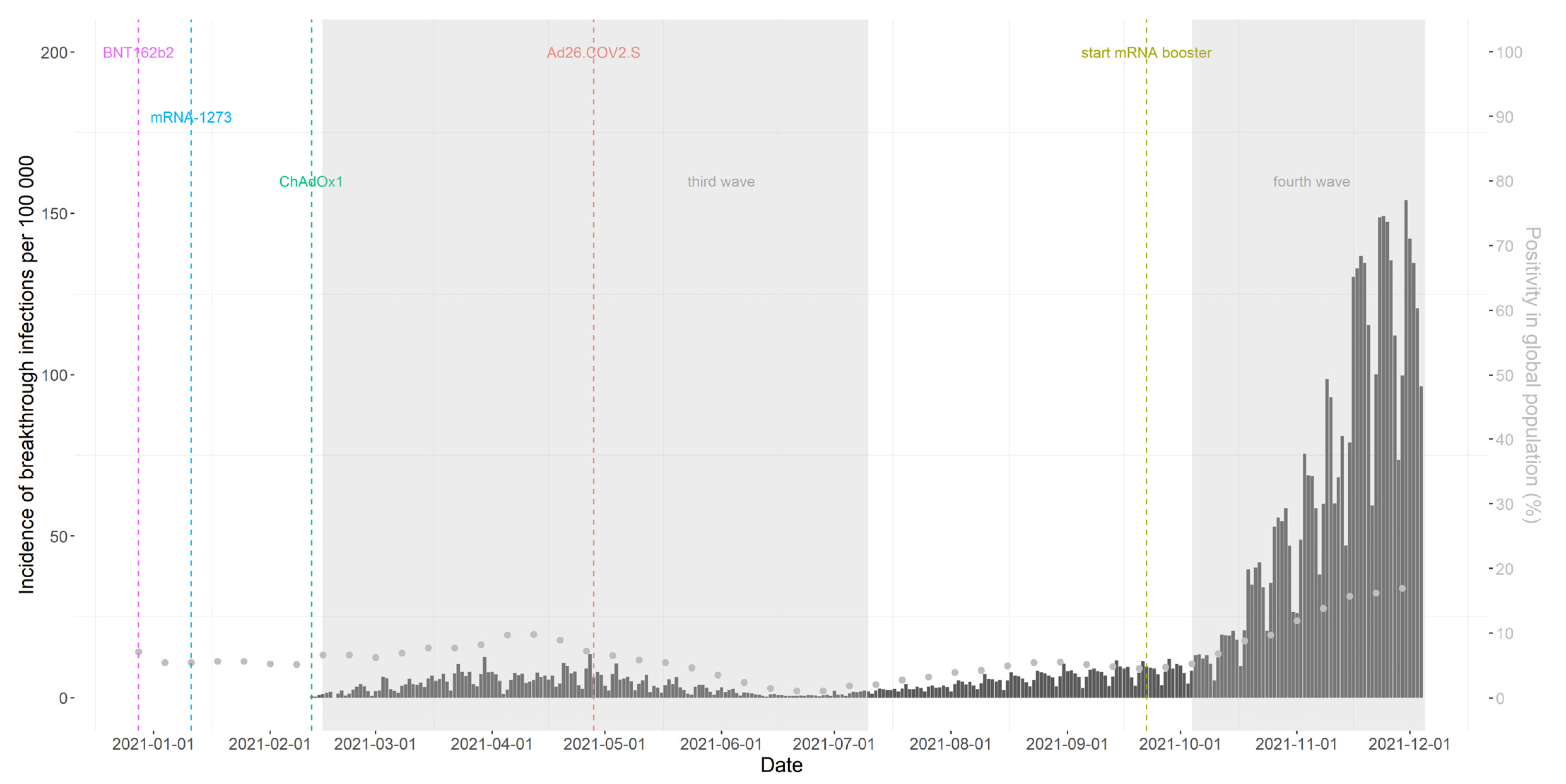
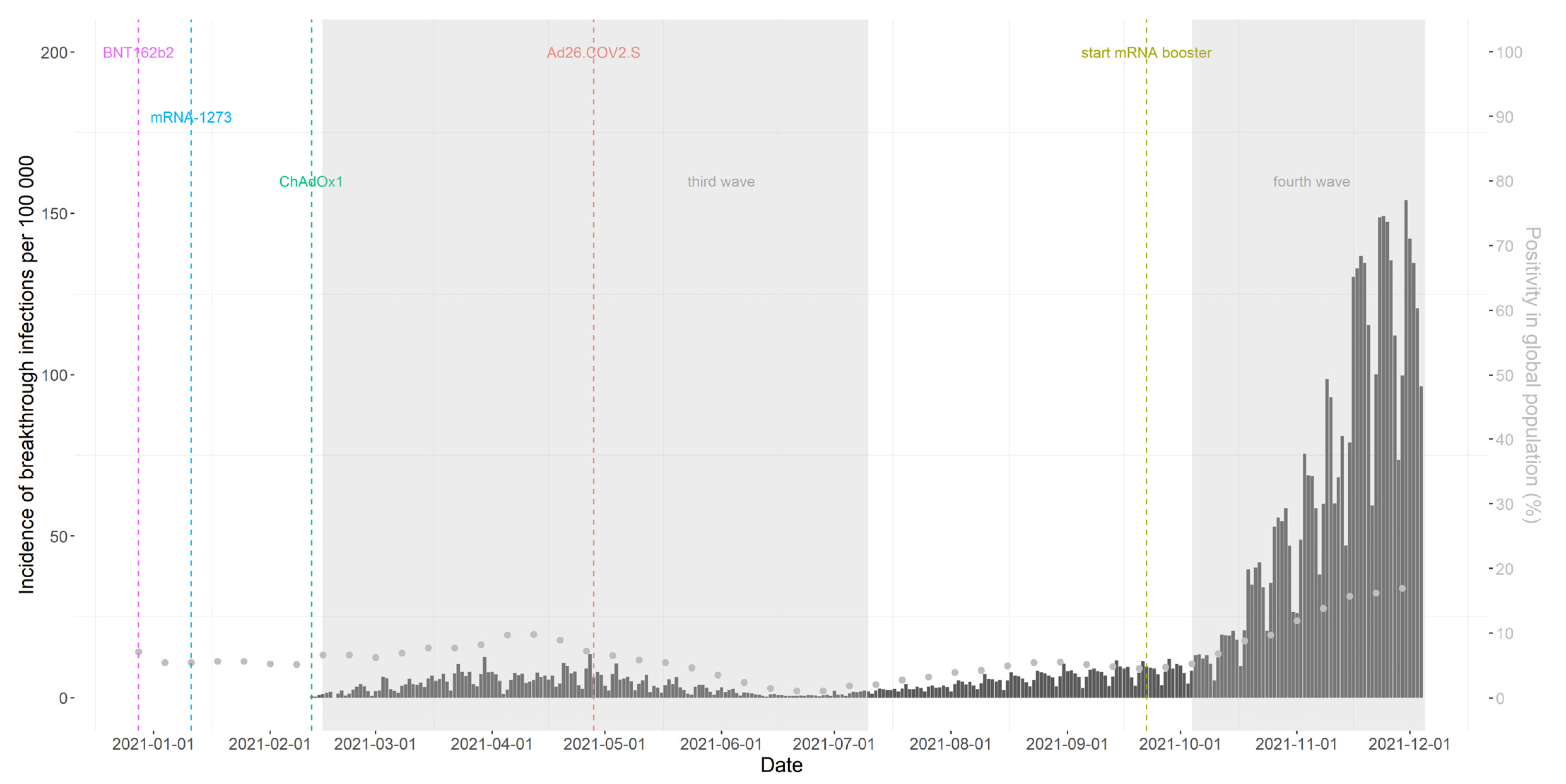
Four different vaccines were used – Pfizer/BioNTech (BNT162b2), Moderna (mRNA-1273), Oxford/AstraZeneca (ChAdOx1) and Janssen (Ad26.COV2.S).
Dr. Veerle Stouten and colleagues at Sciensano, the National Public Health Institute of Belgium, studied the incidence of breakthrough infections – infections that “broke through” the protective barrier of vaccination – for each vaccine brand.
They also investigated the risk factors and symptoms associated with breakthrough infections.
Such information can be helpful when designing vaccination programmes, including decisions about who would benefit most from a booster dose and the timing and type of vaccine to be used.
The study included all people in Belgium aged 18-plus who were fully vaccinated against COVID-19 between February 1 and December 5, 2021. The 8,062,000 participants were followed up for an average of 150 days, from 14 days after their second dose.
4.6% of the participants (373,070) had a breakthrough infection. This figure does not, however, take into account how long each participant was followed-up. When this is factored in, the incidence rate is 11.2 per 100 person-years. This means that if 100 participants were followed up for one year, 11.2 would be expected to develop a breakthrough infection.
The researchers also looked at the factors associated with breakthrough infections. These analyses were adjusted for age, sex, prior COVID-19 infection and a person’s exposure to the SARS-CoV-2 virus through their profession or environment.
Vaccination with a viral vector vaccine (Oxford/AstraZeneca or Janssen) was associated with a higher risk of a breakthrough infection than an mRNA vaccine (Pfizer/BioNTech or Moderna).
The Oxford/AstraZeneca vaccine was associated with a 68% higher risk of a breakthrough infection than the Pfizer/BioNTech vaccine. The Janssen vaccine was associated with a 54% higher risk of breakthrough infection than the Pfizer/BioNTech vaccine.
In contrast, breakthrough infections were 32% less likely to occur in those who received the Moderna vaccine than in those who had the Pfizer/BioNTech jab. (The Pfizer/BioNTech vaccine was used for all comparisons.)
The researchers point out, however, that the study was not designed to carry out a formal comparison of vaccine effectiveness between brands.
There was a higher incidence of breakthrough infections in younger age groups (18-64 year olds) than in older age groups (65-84 or 85-plus year olds), which might be due to differences in social behaviour.
Healthcare workers were 40% less likely to develop a breakthrough infection than non-healthcare workers. This might reflect healthcare workers “good shielding” – high vaccine coverage and intensive use of PPE while at work.
The analysis also found that those with a prior COVID-19 infection before vaccination were 77% less likely to have a breakthrough infection than those who hadn’t had Covid previously.
Of 216,814 breakthrough infections with information available on symptoms, the majority (70.1%) were symptomatic, with rhinitis (a runny nose), a cough and headache the most common symptoms.
Among persons with a breakthrough infection, those with a prior infection were 62% less likely to have symptoms than those who hadn’t had Covid previously.
The study’s authors conclude: “We observed an incidence rate of breakthrough infections of 11.2 per 100 person-years based on a large nationwide Belgian cohort of fully vaccinated persons. This means that if 100 participants were followed-up for one year, 11.2 would be expected to develop a breakthrough infection.”
Dr. Stouten adds: “We identified risk factors associated with breakthrough infections, such as vaccination with adenoviral-vector vaccines, which could help inform future decisions on booster vaccination strategies internationally.
“Moreover, we observed that hybrid immunity of combined prior infection and vaccination not only lowered the risk of breakthrough infections but also of having symptoms when experiencing a breakthrough infection, highlighting its protective effect.
“The majority of the breakthrough infections included in the study occurred during the period when the Delta variant was dominant. We expect to see similar patterns regarding characteristics of breakthrough infections due to the Omicron variant but we need to continue to monitor breakthrough infections and study their severity and multiple recurrences, as well as the role of emerging variants to confirm this.”

