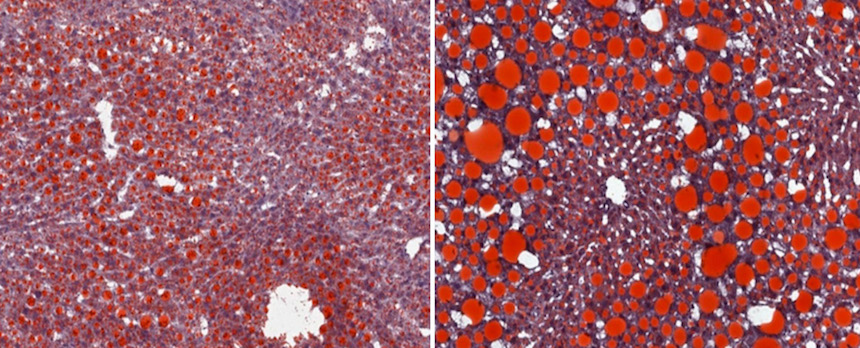
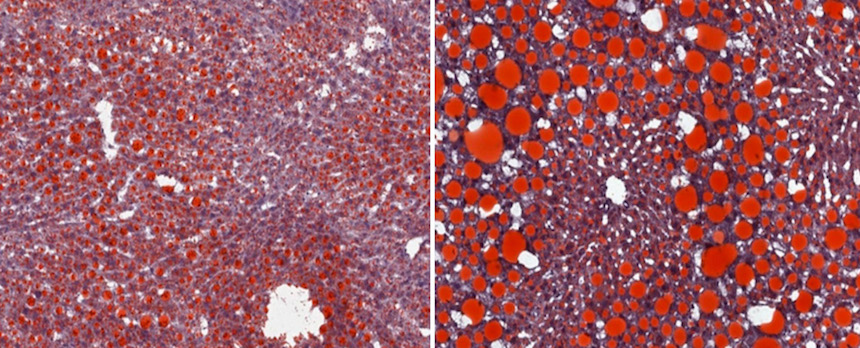
New findings from mouse models reveal that the type of immune response that helps maintain healthy metabolism in fatty tissues, called type 2 immunity, also drives obesity-induced nonalcoholic fatty liver disease (NAFLD). The work, led by scientists at the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, shows that the inflammatory environment in the fatty liver is more complex than previously thought. These insights may inform the development of new NAFLD treatments as well as immune-altering therapies for obesity and related health issues in people with NAFLD.
NAFLD affects an estimated 64 million people in the United States. Over time, it can progress to nonalcoholic steatohepatitis (NASH), eventually leading to liver damage and scarring. NAFLD is a leading indication for liver transplantation.
Although the mechanisms regulating NAFLD progression have been unclear, scientists had suspected that the type of immune response that inflames fatty tissues during obesity, known as type 1 immunity, also worsens liver disease. Unexpectedly, the NIAID-led team found that obese mice engineered to have strong type 1 immune responses were resistant to NASH. This protection was associated with activation of a type 1 immune molecule called IFN-gamma. Obese mice lacking IFN-gamma progressed rapidly to NASH and developed liver scarring.
Further experiments revealed that NASH-induced scarring depends on TGF-beta, a broad immune system regulator and target for experimental NASH therapies, and IL-13, a type 2 molecule produced by various immune cells, including eosinophils(link is external). Blocking TGF-beta in mouse models slowed NASH-driven liver scarring, but the number of eosinophils and amount of IL-13 produced in the liver increased to compensate for the lost TGF-beta function. Simultaneously blocking TGF-beta and IL-13 more effectively stopped liver scarring.
To determine whether these findings may be relevant to human disease, the scientists examined liver biopsies from people with NASH. As in mice, the researchers observed evidence of type 2 inflammation and accumulation of eosinophils.
The researchers next plan to use mouse models to assess the specific roles of eosinophils in the liver and to study ways to specifically block the IL-13 and TGF-beta cell-signaling that leads to liver scarring.

