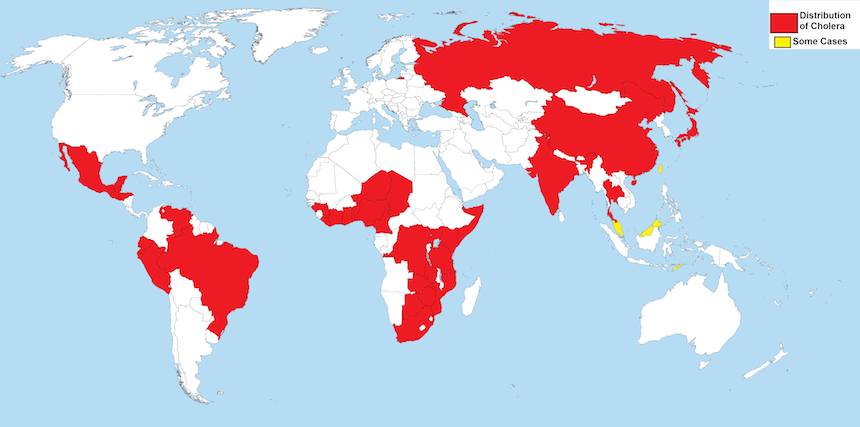
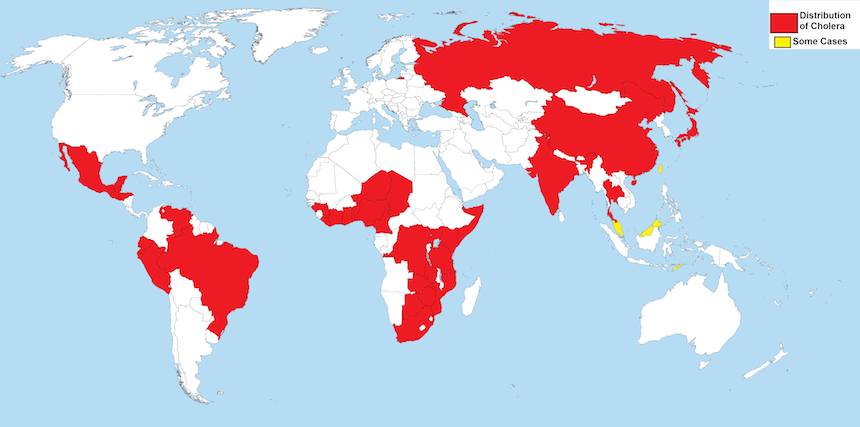
As John Clemens and colleagues describe in a Seminar published recently in The Lancet, cholera is an ancient disease. Endemic in the Ganges river basin, it has caused a series of pandemics since 1817, the most devastating being the seventh pandemic, which began in 1961 and is ongoing. Cholera is a disease steeped in medical history—it was during the third pandemic that John Snow plotted his famous map of Broad Street, and during the fifth epidemic, that Robert Koch sought to identify the causative agent. Spread by the faeco-oral route, the disease affects poor people and the most vulnerable. Cholera is endemic in 47 countries, particularly in areas where the water, sanitation and hygiene (WASH) infrastructure is poor. In these areas, children are particularly at risk. Epidemics occur both within and outside of endemic areas, often amid humanitarian crises, when WASH infrastructure breaks down or is overwhelmed. In situations where the population lacks immunity, a wider age range is affected, often with more severe clinical manifestations. Currently the worldwide cholera burden is high. 60–70% of cholera cases and deaths occur in endemic areas of Africa, which could increase as urbanisation, particularly the growth of slums, places increasing numbers at risk.
Fluid resuscitation as the core of cholera treatment is well established, but recent developments in disease prevention strategies underlie the GTFCC’s roadmap. Improvements in WASH systems can eliminate cholera, but although the rate of return on investment is good, these are initially expensive, and the slow expansion of WASH provision has failed to tackle the burden of cholera and other water-borne diarrhoeal diseases. The pivotal change in cholera control has been the development of oral cholera vaccines (OCV), underpinned by an improved understanding of the mechanism of cholera immunity. In a series of landmark research developments over the past 10 years, the efficacy, safety, acceptability, and feasibility of these vaccines have been demonstrated. The creation of a growing global OCV stockpile by WHO, with long-term funding support from Gavi, signalled the step-change in cholera prevention strategies and, since 2013, 13 million vaccine doses have been deployed, mostly in the emergency control of epidemics.
The novelty of the GTFCC eradication strategy is based on three key axes. First, the emphasis on rapid response to outbreaks: controlling epidemics through community engagement, improved early warning surveillance, and the rapid delivery of cholera control kits, OCV, and WASH supplies. Second, the strategy implements a multisectoral approach in hotspots of endemic cholera. OCV programmes will be used as a bridge, immediately reducing disease burden and mortality while long-term solutions are developed: sustainable WASH infrastructure, strengthened health systems able to anticipate epidemics, and strong community engagement required to stop transmission. The third axis is the coordination of operational support, local and global resourcing, and technical expertise delivered by GTFCC. Over the next 18 months, the task force will support six to eight countries to develop cholera control plans, develop an investment case on cholera, and create operational guidance on integrated prevention strategies ahead of a review meeting planned in 2019.
The bold vision of the Global Roadmap is welcome but the challenges that lie ahead should not be underestimated, Paul Spiegel, director of the Center for Humanitarian Health at Johns Hopkins University told The Lancet. Ending cholera depends both on successful delivery of the prevention strategies on the ground and mitigating risks to the Global Roadmap at a high-level (securing financing, ensuring vaccine availability, and galvanising political will). The technical ability to control cholera is within our capabilities. After 50 years, could the tide be finally turning on the seventh pandemic?
This article published courtesy of The Lancet.

