In findings with potentially important implications for cervical cancer screening, scientists at the National Cancer Institute (NCI)-designated Montefiore Einstein Cancer Center (MECC) have developed a test for detecting a type of cervical cancer that Pap tests often miss. The findings published online today in the Journal of the National Cancer Institute (JNCI).
“Our novel test appears sensitive for detecting cervical adenocarcinoma [ADC]—which now accounts for up to 25% of cervical cancer cases—as well as its precursor lesions, adenocarcinoma in situ [AIS], that often develop into ADCs,” said Howard Strickler, M.D., M.P.H., co-senior and corresponding author of the JNCI paper and a member of MECC.
“Because ADCs are often missed by current screening methods, they have higher mortality rates than the more common cervical squamous cell cancer,” Dr. Strickler added. “Our goal is to catch the disease early, before it develops into cancer.” Dr. Strickler is also professor and head of the division of epidemiology and the Harold and Muriel Block Chair in Epidemiology and Population Health at Albert Einstein College of Medicine.
A Novel Approach to Testing
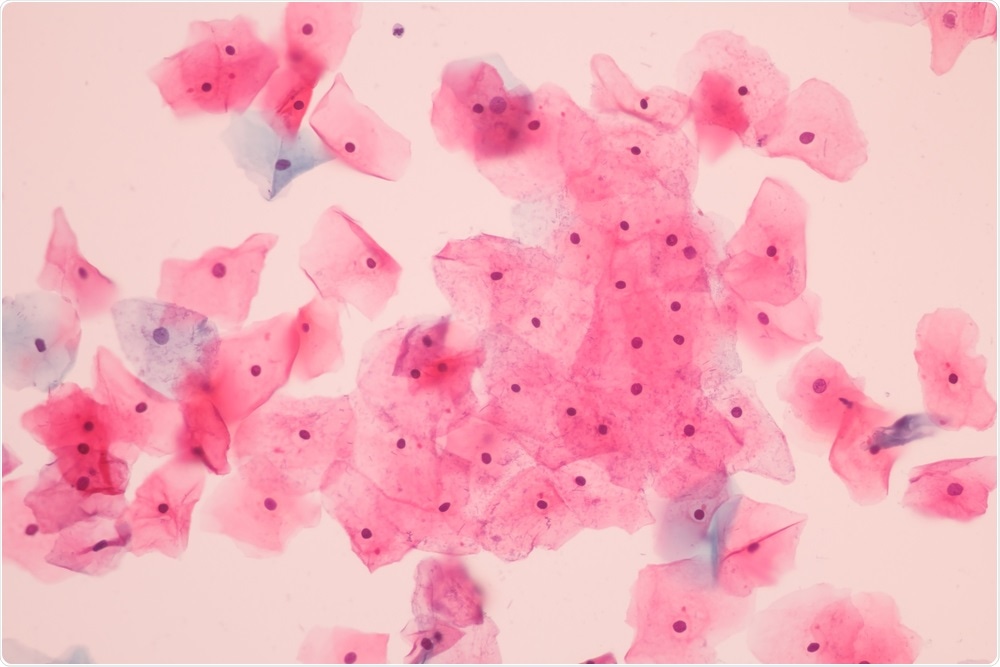
The widespread use of the Pap test, in which a pathologist examines tissue samples for abnormal cells, has significantly reduced the incidence of cervical squamous cell cancer over the past six decades. However, the incidence of ADC has not decreased, probably because the Pap test is less effective at detecting it.
In recent years, testing for human papillomaviruses (HPVs)—which cause virtually all cases of cervical cancer—joined the Pap test as a standard screening tool for cervical cancer. Although there are more than 100 types of HPV, three types—HPV 16, 18, and 45—account for more than 70% of all cervical cancer cases and more than 90% of ADC cases. The current HPV tests cover all three types and can alert infected women that they face a high risk for developing cervical cancer. While vaccines for preventing cervical cancer—including Gardasil-9, which protects against nine HPV types—are safe and effective, several generations of women are above the age for receiving the vaccine. Therefore, screening and treatment for prevention of cervical cancer will remain critical for decades to come.
The MECC-developed HPV test assessed HPV 16, 18, and 45 in a novel way: by specifically looking at methylation levels. “The advent of next-generation genetic testing has opened up opportunities for us to more accurately detect oncogenic HPV strains and patterns in the genomes that correspond with the development of AIS and ADC,” said Robert D. Burk, M.D., professor of pediatrics, of microbiology & immunology, of epidemiology and population health, and of obstetrics & gynecology and women’s health at Einstein and MECC member, who co-led the study.
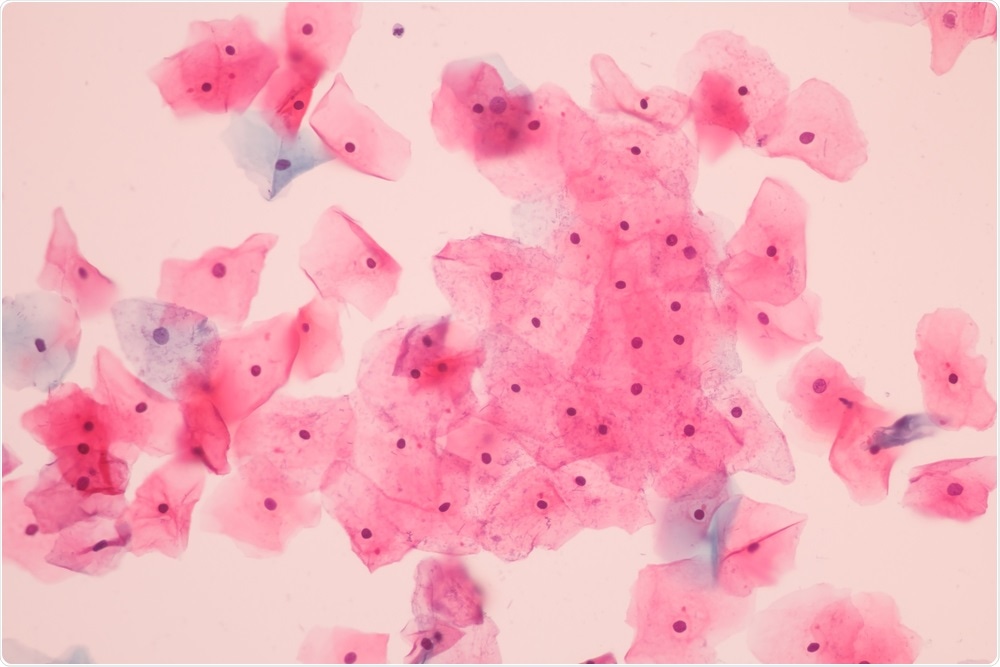
Methylation—the addition of methyl (CH3) groups to a region of DNA—is a routine occurrence in DNA, both viral and human, and plays a critical role in altering gene expression. The JNCI study, a collaborative project with the NCI, part of the National Institutes of Health, investigated methylation levels in cervical tissue samples from 1,400 women who had undergone cervical cancer screening at Kaiser Permanente Northern California before 2014 and whose cervical cancer status was known.
In assessing the HPVs in the cytological samples, the researchers tallied up the methylation percentages for each of 35 different viral-genome sites, with each sample receiving a final “methylation score” equal to the average methylation percentage across all 35 sites. Those women with methylation scores in the upper 25% had very high odds for having developed either ADC or AIS.
“Our findings, if confirmed by clinical trials, suggest that women with a high methylation score may benefit from colposcopy and specialized tissue evaluation, beyond just a Pap test, which could lead to early diagnosis and treatment for ADC or the removal of AIS lesions before they develop into ADC,” said Dr. Burk.
Improving Equity in Cervical Cancer Screening
“Given that our test uses equipment that could be simplified, it has the potential to expand testing in lower-resourced countries,” said Dr. Strickler, who has long studied HPV in women living with HIV, who are more likely to acquire an HPV infection.
Cervical cancer remains the fourth most common type of cancer in women, with the burden significantly higher in lower- and middle-income countries, including those in Sub-Saharan Africa, where HIV-HPV coinfections are common. There are also significant disparities within the United States. In New York City, rates of cervical cancer in the Bronx, which is home to the poorest urban congressional district in the country, are 50% higher than in Manhattan. More frequent and effective screening could help address this health disparity.
“Ideally, the new HPV methylation test would only need to be done once every three to five years,” said Dr. Strickler. “We are hopeful that this test will be able to increase cervical cancer screening equity in the U.S. as well.”

