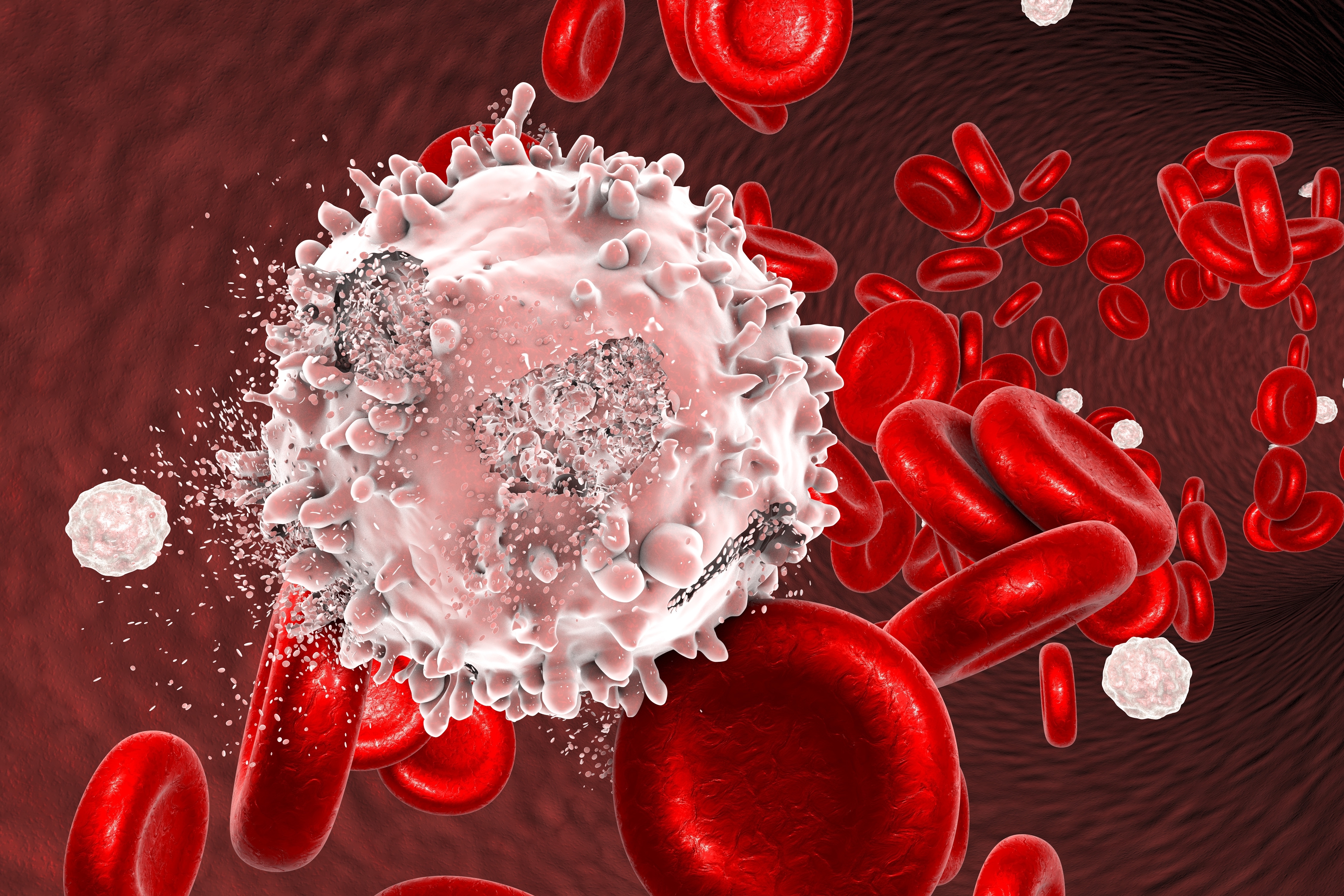
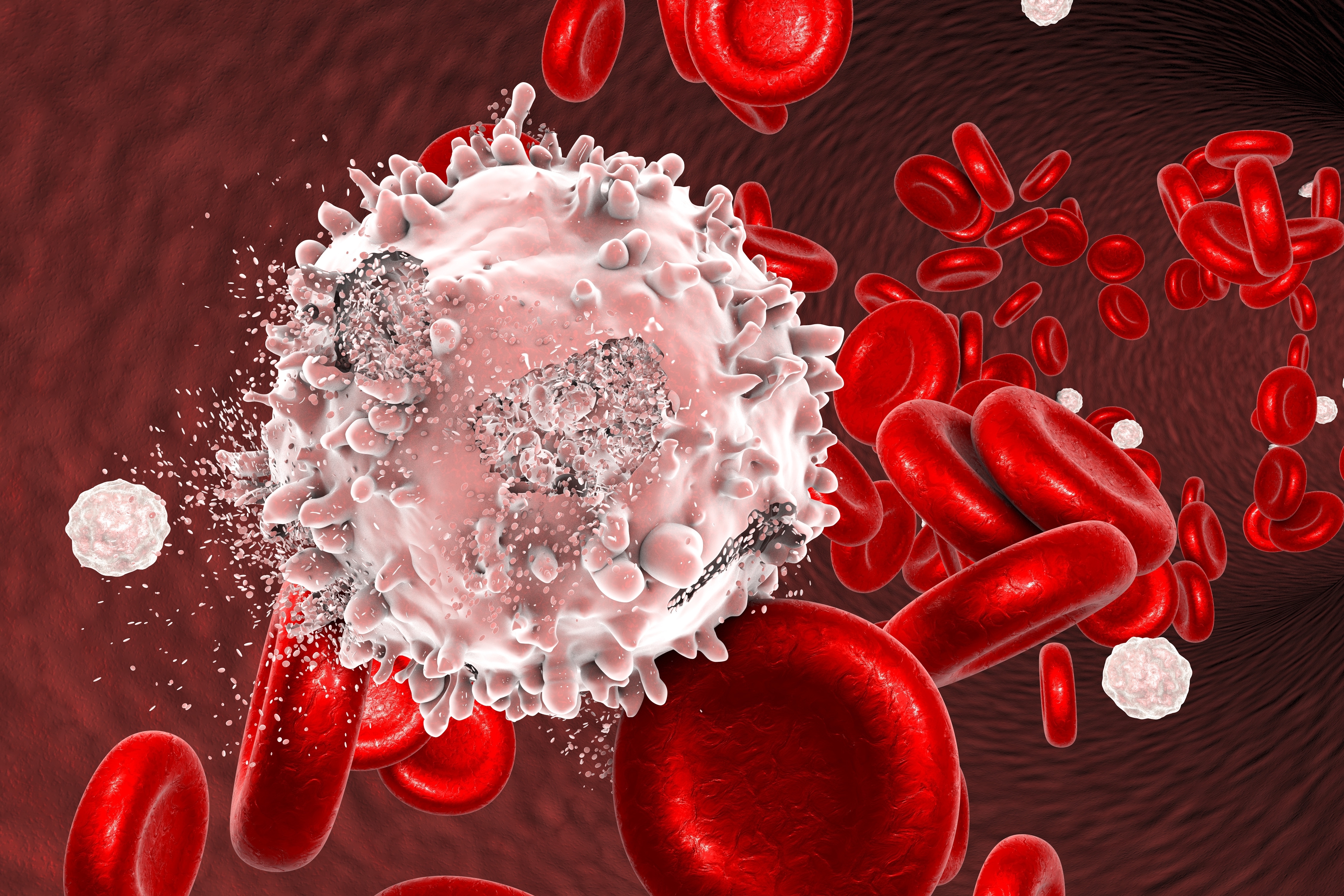
The advent of T-cell therapies, where cells of the immune system are directed towards malignant cells, has changed the treatment paradigm of certain forms of blood cancer. However, despite the huge progress in this field, not all patients affected by blood cancers benefit from these therapies, while many may experience serious side effects. Researchers are therefore looking into other types of immune cells for answers. NK cells patrol our system, looking for abnormal cancerous or virally infected cells, and once they find their suspects, they destroy them. These cells are now in the spotlight as they may be exploited as a novel treatment approach and overcome some of the challenges with T-cell therapies.
How are cancer cells escaping their killer?
The immune system, including NK cells, protects our body from malignant cells. However, cancer cells have found ways to escape their own death by the immune system. Previous studies have identified some factors regulating the sensitivity of tumor cells to NK cell-mediated killing, but very little is known about blood cancers.
“Our goal was to thoroughly evaluate the resistance and sensitivity mechanisms to NK cell therapies across blood cancers,” says physician-scientist Olli Dufva from the University of Helsinki.
To achieve this, the researchers used a method known as single-cell RNA sequencing, a powerful technique that has emerged in the last decade. Although each cell of an organism contains the same DNA (except for mutations), only a precise set of genes is activated at a given time in a certain cell and gets transcribed to RNA. Single-cell RNA sequencing tells us which genes are active in each individual cell and is considered the current gold standard for defining the states of cells at the molecular level.
“The genes expressed in different tumor or immune cells are quite well known, but they do not tell the whole story,” adds Dufva. “These cells interact, and they induce changes in the activity of each other’s genes.”
The team of scientists exposed different types of cancers, including leukemias, lymphomas, and myelomas, to NK cells in the laboratory. Upon interaction, they evaluated the activity of genes in both NK and cancer cells at single-cell resolution.
“We found that NK cells do not react similarly to all cancer cells: some cancers cause the NK cells to activate and destroy the cancer cells, while others do not induce any response,” says PhD Sara Gandolfi, physician-scientist who conducted research for this project in both the Mustjoki and Mitsiades Labs in Helsinki and Boston, respectively.
New therapeutic targets to tackle resistance of blood cancers to immune cells
How could resistant cancer cells be sensitized to immune attack? Using the CRISPR-Cas9 gene editing method, the researchers were able to systematically turn on or off genes in the cancer cells. They then measured which alterations made the cancer cells more easily killed by NK cells.
“We uncovered several genes involved in the sensitivity and resistance mechanisms to NK cells,” continues Gandolfi, “including both already known mechanisms (antigen presentation and death receptor regulators) and new, previously unappreciated culprits (adhesion-related glycoproteins, protein fucosylation genes, transcriptional regulators).”
The proteins produced by these genes could be targeted by different types of treatments, such as antibodies, which could lead to improved cancer immunotherapies in the future.
“Our study provides a comprehensive picture of the molecular changes happening in NK and blood cancer cells upon interaction and highlights the underlying mechanisms of sensitivity and resistance to NK cell-mediated killing. This is an important resource for researchers studying blood malignancies to develop new personalized NK cell immunotherapies,” concludes Professor of Translational Hematology Satu Mustjoki (University of Helsinki and Helsinki University Hospital Comprehensive Cancer Center).
“This study identified many factors are involved in NK cell resistance commonly across hematologic neoplasias, as well as other molecules that have distinct roles for individual groups of blood cancers. This highlights the value of studies such as ours which seek to understand the mechanisms responsible for immunotherapy resistance across several different types of cancers,” adds Associate Professor Constantine Mitsiades (Dana-Farber Cancer Institute, Harvard Medical School).

