For women with breast cancer, breast-conserving therapy (BCT) is associated with improved sexual well-being, compared to mastectomy followed by breast reconstruction, reports a study in the March issue of Plastic and Reconstructive Surgery®, the official medical journal of the American Society of Plastic Surgeons (ASPS). The journal is published in the Lippincott portfolio by Wolters Kluwer.
“In our study, patients undergoing BCT scored consistently higher on a measure of sexual well-being, compared to total mastectomy and breast reconstruction,” comments Jonas A. Nelson, MD, MPH, of Memorial Sloan Kettering Cancer Center, New York. “The findings highlight the need for increased attention to sexuality when discussing breast cancer treatment options.”
Sexual well-being after breast cancer surgery
Many women with breast cancer have sexual health concerns. In previous studies, up to 85% of breast cancer patients report sexual dysfunction but few receive any medical guidance for sexual dysfunction.
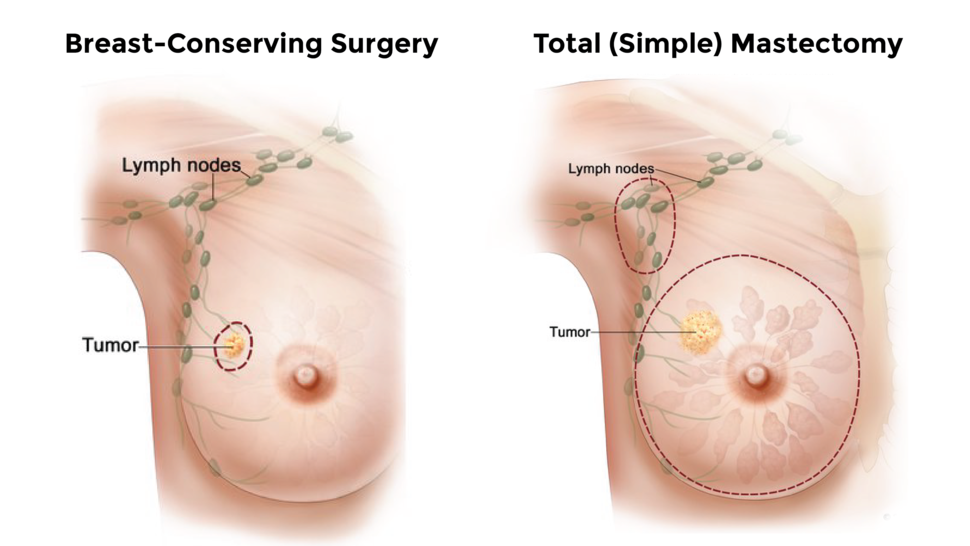
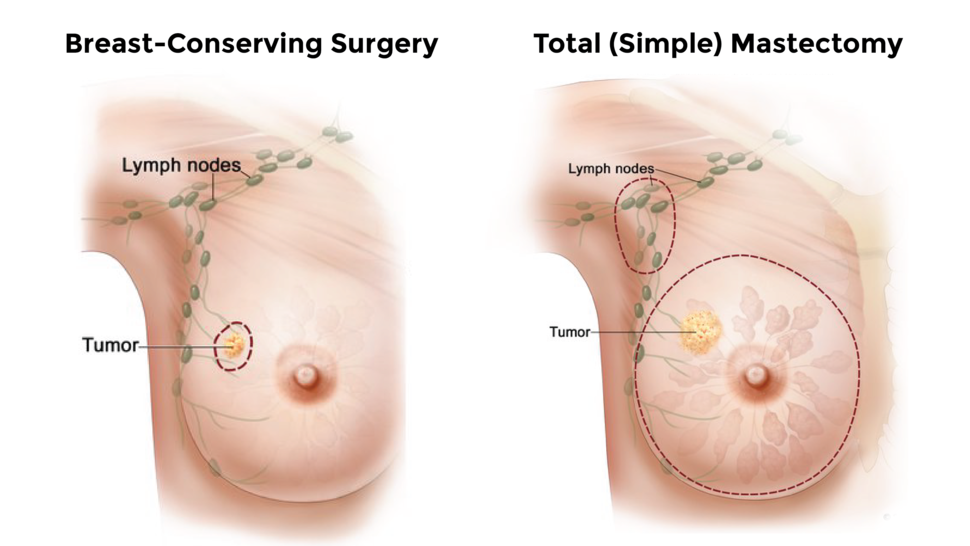
For many patients, BCT – sometimes called “lumpectomy” – offers an effective alternative to mastectomy. For those who undergo mastectomy, breast reconstruction has established benefits in terms of quality of life and self-esteem.
Few studies of breast cancer treatment have focused on sexual well-being, especially in comparing the outcomes of BCT versus postmastectomy breast reconstruction (PMBR). Using validated BREAST-Q questionnaire, Dr. Nelson and colleagues analyzed sexual well-being scores for 15,857 patients who underwent breast cancer surgery between 2010 and 2022.
About 54% of patients underwent BCT and 46% had PBMR. Scores on a sexual well-being subscale – addressing sexual attractiveness, sexual confidence, and comfort level during sex – were compared between groups, including long-term follow-up when available.
Better recovery after BCT; few patients receive sexual medicine consultation
Before surgery, the two groups had similar average scores for sexual well-being: 62 in the BCT group and 59 in the PBMR group (on a 0-to-100 scale). By six months, sexual well-being score in the BCT group had improved to 66, and remained around that level at up to five years.
At all times, women undergoing PBMR had lower sexual well-being scores, compared to BCT. Average score at six months was 49, improving to 53 with longer follow-up. Sexual well-being score was even lower – average 41 – for patients who had not yet completed breast reconstruction by the end of the study period.
Overall, scores averaged 7.6 points higher in the BCT group. Sexual well-being was significantly correlated with scores in other BREAST-Q domains, including physical well-being of the chest, satisfaction with breasts, and psychosocial well-being.
Despite the impact on sexual well-being, only 3.5% of the BCT group and 5.4% of the PBMR group received sexual medicine consultation, which was available from a dedicated service at the authors’ cancer center. After adjustment for other factors, PBMR patients were about half as likely to receive sexual medicine consultation.
The study adds to previous evidence that women undergoing BCT for breast cancer recover sexual well-being more quickly, compared to PMBR. “For breast cancer patients who are eligible for either BCT or mastectomy, BCT may be the superior choice for patients who wish to maintain their sexual well-being,” the researchers write.
The authors also emphasize the need to consider and discuss the impact of breast cancer surgery on sexual well-being. Dr. Nelson concludes: “Although many patients have low sexual health, most do not receive sexual medicine consultation, suggesting an opportunity for providers to improve breast cancer patients’ sexual health.”

