COVID-19 is known primarily as a respiratory disease, with symptoms that include cough, shortness of breath, and, in severe cases, acute respiratory distress syndrome and pneumonia. Now, researchers from Cleveland Clinic’s Department of Biomedical Engineering note in a recent review that infection with the coronavirus may also affect the central nervous system and cause corresponding neurological disorders, including ischemic stroke, encephalitis, encephalopathy and epileptic seizures.
According to the review–published in Cells and authored by Chaitali Ghosh, PhD, and Aneesha Achar–the symptoms of COVID-19-related neurological manifestations include dizziness, headache, a loss of consciousness and ataxia (loss of balance and muscle control).
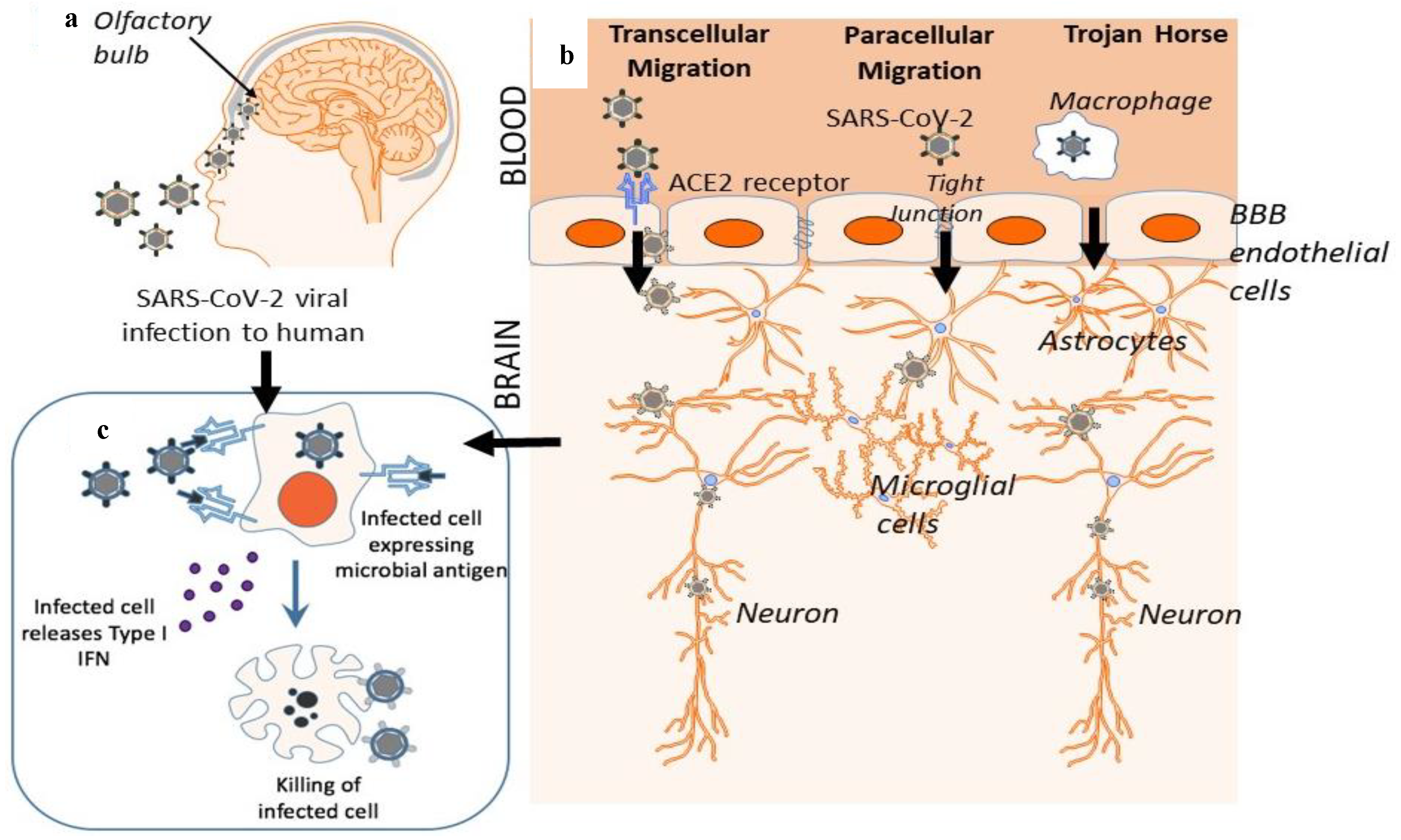
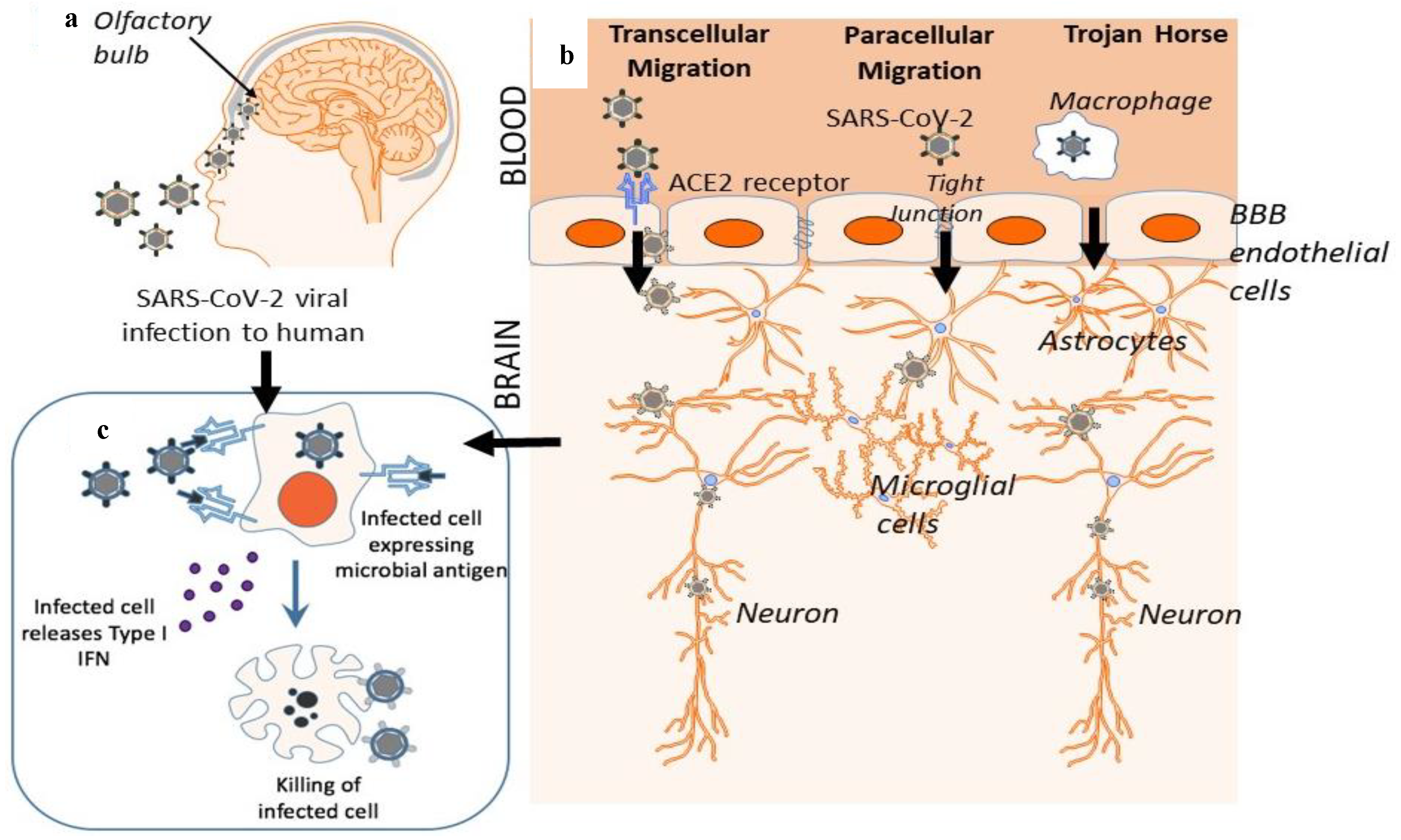
The coronavirus gains access to the body by attaching to a specific receptor most abundantly found on cells that line many organs and tissues throughout the respiratory system, called the ACE2 (angiotensin-converting enzyme 2) receptor. ACE2 can be found less abundantly on cells in other areas of the body–including the heart, esophagus, kidneys and bladder–which increases the chances of viral infection, including through the central nervous system.
As reported in the review, the coronavirus may enter the central nervous system either through a porous bone in the nasal cavity (which causes the loss of smell and/or taste commonly experienced with COVID-19), or through the body’s circulatory system, subsequently crossing the blood-brain barrier.
“Ordinarily, the blood-brain barrier allows nutrients to reach the brain while protecting it from circulating toxins or pathogens that could cause infections,” Dr. Ghosh said. “However, the exact mechanisms underlying COVID-19-associated neurological disorders remain unknown. Such viral infectivity could alter blood-brain barrier function, which may influence disease progression.”
Cytokine storms: An early warning system
Once in the central nervous system, the virus activates proteins called cytokines (central players in the body’s immune response) and initiates a “cytokine storm.” This can cause inflammation in the central nervous system and affect blood-brain barrier integrity.
What’s more, while cytokine storms are usually associated with severe cases of COVID-19, Dr. Ghosh sounded a note of warning. “Central nervous system disorders can occur in patients who have only mild or moderate COVID disease,” Dr. Ghosh said. “In fact, they can also come about even before the patient has any respiratory symptoms.”
While there is currently limited evidence on long-term consequences of COVID-19-associated neurodegenerative and inflammation-mediated brain diseases, investigations into whether these comorbidities are risk factors for COVID-19 would be critical to follow.
“I am eager to define and learn more about which signaling pathways are linked to which neurological disorders, and think this will be an exciting new frontier in COVID-19 research,” said Dr. Ghosh

