

The number of children who die before reaching their fifth birthday is closely monitored as a marker of social well-being and national development. It best summarises the social, economic, environmental and health care systems that children are born into and thus used as the basis of planning health strategies, programmes and interventions. It’s also an important tool for evaluating the success of a country’s child health policies.
There has been remarkable progress in improving child survival over the last three decades. But there’s a long way to go: globally, 5.4 million children died before reaching their fifth birthday in 2017. This is equivalent to 15,000 child deaths per day. And the burden is unevenly distributed: sub-Saharan Africa region recorded 14 times more of these deaths compared to high-income countries. The region is home to all six countries in the world that recorded child mortality rates above 100 deaths per 1000 live births.
Kenya performed well above average, with a rate of 46 deaths per 1,000 live births compared to an average of 76 across sub-Saharan Africa region.
Our Kenyan study set out to estimate child mortality rates in each of the country’s 47 counties every year since 1965. This allowed us to explore changes over time, disparities in child survival by county and progress and gaps towards achieving global targets of 2000 and 2015 at different times over the last 30 years. We achieved this by assembling all mortality related data in Kenya and applied a range of techniques to generate child mortality rates.
The findings suggest that, while national trends may be useful for regional and global policy advocacy, they can also be misleading. This is because within-country differences are masked by the national aggregate levels of child mortality.
Identifying counties where mortality remains higher than the national average is valuable for at least two important reasons. It can lead to governments properly directing suitable interventions that are most likely to bring down child mortality rates. It can also ensure effective and equitable resource allocation to reduce inequalities. This is specifically relevant to Kenya where health is now managed by county governments.
What we found
Our findings showed that, shortly after independence in 1963, one in every seven Kenyan children born alive, died before the age of five. More than five decades later, mortality has declined significantly. But it remains high, with one in every 19 children not reaching their fifth birthday. The overall decline over this period was 62% but it was uneven over time.
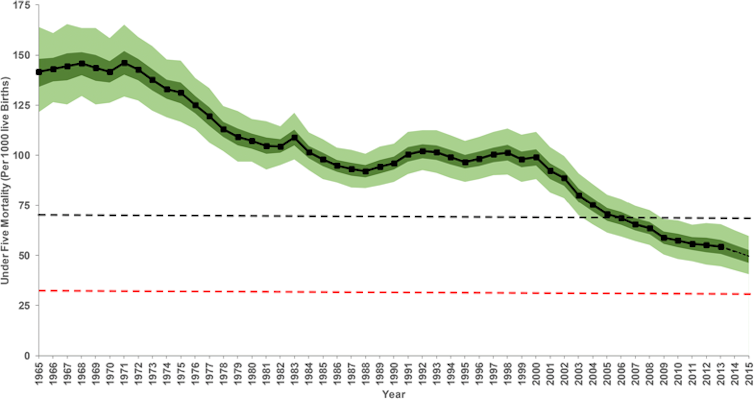
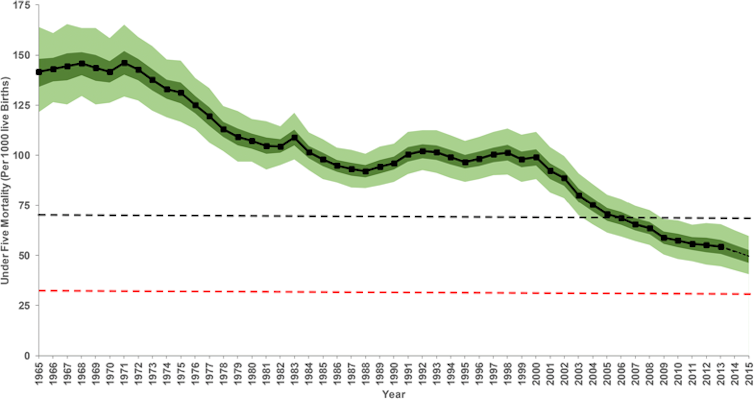
We found that the rate declined steadily from the early 1970s to late 1980s and again from early 2000 to 2013. But there was stagnation or reversal between these declines during the 1990s. More alarming is that Kenya fell short of the 2000 milestones set during the world summit for children aimed at reducing child mortality by a third (1990-2000) or to 70 deaths per 1000 live births by 2000 and only managed a 48% reduction against a target of 67% in the millennium development goal 4 monitoring period (1990 to 2015).
County-level results showed that in 1965, 11 counties – mainly in coastal or arid and semi-arid areas – had mortality rates over 200 per 1000 live births. During this time only four counties had rates below 75 deaths per 1000 live births.
Over 50 years, there have been significant reductions. But the success has been variable, with reductions ranging between 19% and 80%. Counties with high mortality in 1965 witnessed massive declines compared to counties that had lower starting rates, but these same high mortality counties still had the highest rates of mortality in 2013. By 2013 there was a 3.8 times difference between high mortality and low mortality counties, a reduction from five-fold in 1965.
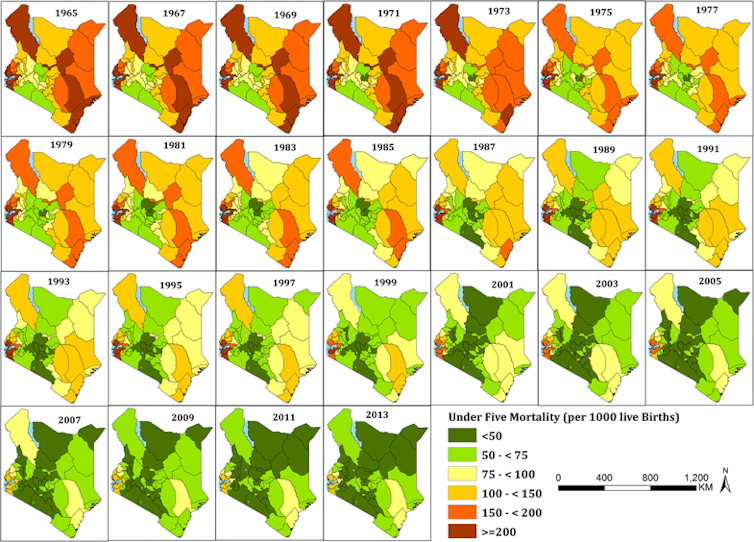
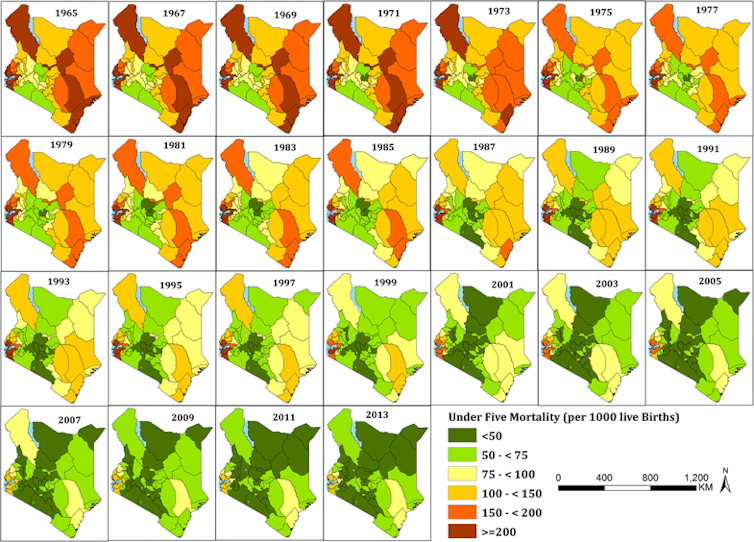
Finally, the results showed that at the county level, Kenya performed sub-optimally in meeting the goals set during the world summit for children for the period 1990 to 2000. Only 25, or half of all counties, achieved the 2000 goals by reducing child mortality to a rate less than 70 or by a third.
More worrying is that no county achieved the goals under millennium development goal 4 by 2015.
Set local targets
These findings come at a time when Kenya has launched further initiatives to improve child survival and populations well being. Most notable is the universal health care programme. It aims to provide individuals and communities with access to health services they need without suffering financial hardship. This is expected to reduce inequalities and will need to be monitored.
In the current decentralised form of governance, all the 47 county governments have been keen to set local targets to monitor and reduce child mortality through county integrated development plans and statistical plans. Our results are invaluable for setting informed baselines and tracking local county specific goals as well as the 2015 sustainable development goals framework. Goal 3.2 of this framework partly aims to reduce child mortality to at most 25 deaths per 1000 live births by 2030.
At the national level, the allocation and distribution of health related resources could be better informed through these findings.
Counties need to focus on rolling out targeted packages of intervention tailored to individual contexts, alongside existing interventions, if they are to record further declines.![]()
![]()
Peter Macharia, PhD Candidate: The Open University UK and, Kenya Medical Research Institute and Emelda Okiro, Head, Population Health Unit, KEMRI, Kenya Medical Research Institute
This article is republished from The Conversation under a Creative Commons license.

